Neonatal Brachial Plexus Palsy (NBPP) manifests as arm weakness (with passive range of motion greater than active) and loss of sensation, evident early in life due to stretching or compression of the nerves of the brachial plexus.
Causes and Symptoms
The nerves of the brachial plexus may be affected during development in the uterus or during the descent and emergence of the fetus from the uterus and pelvis with maternal pushing and naturally expulsive forces. Biomechanically, nerve injury can result from exogenous forces (clinician-applied) or endogenous forces (natural physical events move the fetus from the uterus through the birth canal and out of the maternal pelvis). No consistent data exist to demonstrate that either isolated exogenous or endogenous forces cause NBPP, but the available data do suggest that the occurrence of NBPP may be a multifactorial event. NBPP occurs with an approximate incidence of 1.5 cases per 1000 live births, with or without shoulder dystocia at the time of both vaginal and cesarean delivery. Although many risk factors have been reported, only shoulder dystocia is a statistically significant clinical predictor for NBPP.
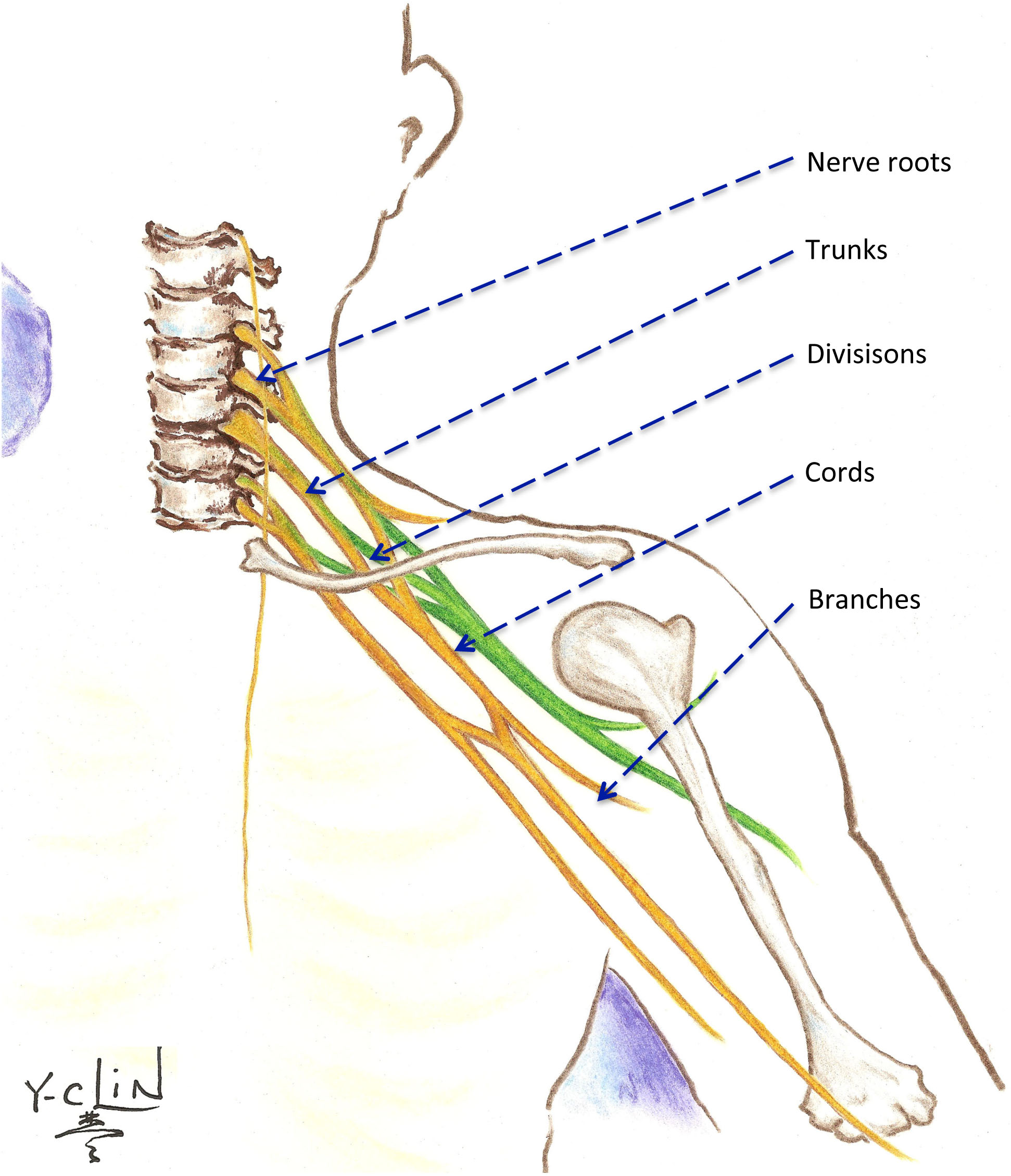
All cases of NBPP are not the same, and the clinical presentation may be radically different depending on which nerve zones of the brachial plexus are affected. The intricate intersecting nature of the brachial plexus implies that thousands of potentially different palsies can ensue, but in reality, only a few variations actually occur. The most useful classification scheme for clinical presentation of NBPP is the Narakas Grading system that represents the extent of the spinal nerve root injury: only C5 and C6 nerve roots are injured in Grade 1, C5, C6, C7 nerve roots in Grade 2, and C5 through T1 injured in Grade 3 (without Horner’s syndrome manifesting as eyelid drooping and abnormal constriction of the pupil of the eye) and Grade 4 (with Horner’s syndrome). When this classification system is used in 2-4 week old affected babies, it may prognosticate spontaneous recovery of up to 90% of the patients with Grade 1 NBPP regain functional use of the affected arm whereas <5% of the patients with Grade 4 NBPP regain functional use without medical and/or surgical intervention. The severity of each Narakas Grade can vary from mild conduction block to complete transection of the nerves of the brachial plexus.The brachial plexus is a very complex structure that connects the spinal nerves in the neck to their terminal branches in the arm, supplying motor and sensory function. It is commonly divided into 5 anatomical zones: (1) spinal nerve roots (C5, C6, C7, C8, and T1), (2) trunks (upper, middle, and lower), (3) divisions (anterior and posterior) of each trunk, (4) cords (lateral, posterior, and medial), and (5) branches (terminal). For simplicity, the nerve roots can be indexed to the muscles in the following fashion: C5-shoulder movement, C6-elbow flexion, C7-elbow extension, C8/T1-hand and finger movement. Other classification systems are based on the practitioners that described the specific NBPP cases. Erb’s palsy is commonly used as synonymous to NBPP, but formally, it is an “upper” plexus palsy specifically involving C5, C6, and sometimes C7 spinal nerve roots: this type of NBPP is the most common type and is visually recognized by the “waiter’s tip” posture with the arm adducted, shoulder internally rotated, wrist flexed and fingers extended resulting from loss of both shoulder control and elbow bending. Contrastingly, Klumpke’s palsy is a “lower” plexus palsy that is extremely rare: this type of NBPP can be recognized by a flaccid hand in the context of an otherwise active arm. Total plexus palsy or pan-plexopathy is equivalent to Narakas Grade 3 and 4 and is recognized by a flail arm with or without an ipsilateral drooping eyelid.
Treatment and Therapy

A weak arm observed in the perinatal period warrants confirmation of the diagnosis of NBPP by a specialist. A thorough family, maternal, and perinatal history provides the appropriate context for the physical examination and may support the diagnosis. In the early days after birth, any associated skeletal injuries or fractures should be confirmed by clinical and radiographic evaluation since these injuries may preclude early occupational/physical therapy. No substantial evidence exists to support further injury to the brachial with gentle handling of the neck and affected arm, and immobilization of the arm is not recommended except in the context of skeletal injuries. Determination of the extent and severity of the nerve injury is critical for prognostication and for determination of subsequent treatment. Other neurologic disorders occurring concurrently with NBPP can be suspected with the presence of a lack of spontaneous movements and normal reflexes that suggest global neurological deficits. Alternatively, an observed asymmetric expansion of the chest cavity and difficulty with breathing or feeding can suggest diaphragmatic palsy resulting from associated phrenic nerve injury, confirmed with plain X-rays or ultrasonography; diaphragmatic palsy can be a dangerous condition leading to respiratory distress and early failure to thrive, and if diagphragmatic palsy is present, the condition should be addressed promptly.

With regard to the movement of the affected arm, the treating physician should assess the passive and active range of motion of the affected arm. Available assessment scales of motor function in NBPP can be used to determine the extent and severity of nerve injury, to prognosticate potential functional recovery, and to guide and assess the outcomes from further treatment. Traditional assessments focus solely upon the affected arm, but more recently, assessment methods are refocusing upon the overall function of the child in the context of a weak arm. Supplementing the physical examination with electrodiagnostic (EDX) / electromyographic (EMG) and radiographic (magnetic resonance imaging, MRI, ultrasound, CT) findings are helpful to decide whether nerve reconstruction will be beneficial. Early referral (as soon after birth as possible) of babies with severe or extensive NBPP to interdisciplinary specialty clinics can improve overall functional outcomes as the baby grows. Regardless of the need for surgical intervention, rehabilitation management is critical. Occupational/physical therapy to maintain the normal passive range of motion in all upper extremity joints (especially shoulder external rotation and forearm pronation and supination) facilitates successful functional recovery of global function and timely achievement of developmental milestones. Parents and caregivers should consider themselves to be the patient’s primary therapist by performing range of motion exercises regularly, with multimedia assistance if available several times during the day. Reinforced use of the affected arm while constraining the normal arm (constraint therapy) can aid the child’s recognition of the arm and strengthen the arm through increased arm use during age-appropriate activities. Normal childhood developmental milestones must be monitored. Torticollis can be ameliorated by stimulating neck rotation towards both sides. Similarly, subsequently acquired plagiocephaly can by avoided by promoting symmetrical development of the head by following the adage of “back to sleep, tummy to play." Splinting may be used during sleep to avoid the formation of contractures or to protect floppy joints. As the child grows and formal therapy becomes mundane and discarded, recreational activities like swimming, dance, sports, and more recently, experimental therapist-designed video game platforms can help to sustain the goals of formal occupational/physical therapy.

For NBPP patients who do not recover with conservative management, surgery for nerve reconstruction may be an option, usually occurring between 3-9 months of age. Although the indications and timing for nerve reconstruction have not been absolutely established, most practitioners agree that babies with the extensive total brachial plexus palsy and those with the severe Erb’s palsy will benefit from nerve surgery. The goal of nerve reconstruction is not to regain a normal arm, but surgical intervention is a step towards a functional arm with adequate movement for activities of daily living, if not power. Nerve repair using autologous nerve graft and/or nerve transfer constitute the primary options for reconstructing the brachial plexus. As nerve repair and transfer rely upon regrowth of the normal portions of the nerve through the residual pathways after the injured distal nerve is cleared away (Wallerian degeneration) and as this nerve regeneration is very slow, the ultimate functional outcome from nerve reconstruction surgery may not be apparent for 1-3 years. Toddlers and older children with incomplete recovery following nerve reconstruction or conservative treatment may have functional limitations because of residual muscle weakness and soft tissue contractures, especially around the shoulder and elbow. Radiographic imaging can guide the decision to pursue orthopedic intervention. Internal rotation contractures of the shoulder are very common and can be associated with progressive glenohumeral joint deformity and shoulder joint instability. The indications for surgical intervention include persistent internal rotation contractures despite aggressive non-surgical therapy, progressive joint deformity, and frank dislocation. Surgical options include muscle lengthening with or without tendon transfers, corrective osteotomies, and/or open or arthroscopic reduction of the shoulder joint.

For children with residual elbow, forearm, and hand problems, secondary procedures by a hand surgeon may help function. These procedures include soft tissue releases, joint fusions, muscle transfers, and corrective osteotomies. The usual age for secondary reconstruction of the elbow/forearm function is 4-6 years of age, and for wrist/hand function is 6-13 years of age. Restoration of elbow flexion is a main priority, and in children with a flail wrist/hand, the order of priority is restoration of wrist extension, thumb flexion, finger flexion, followed by thumb and finger extension. For all surgical interventions, the most important factor in producing the optimal result is a cooperative child with intense investment from assertive parents/caretakers. The parents must understand the objectives of the surgical procedures and work diligently with their children in post-operative rehabilitation -- by being their children’s primary therapists. Surgery alone without subsequent rehabilitation management and therapy with parental diligence is unlikely to yield the desired outcome.
Outlook
Overall, the majority of infants with NBPP have a good prognosis for recovering adequate functional use of the affected arm, with rehabilitation management and therapy supplemented with surgical intervention when and where appropriate and desired. Early occupational/physical therapy supports the spontaneous recovery of function and minimizes consequent musculoskeletal comorbidities. Despite the similar incidence of NBPP to cerebral palsy, public awareness and research of this perinatal disorder and its lifelong implications (medical and psychosocial) for the more extensively/severely affected children are significantly lacking. Therefore, our program exists not only to find new medical treatment techniques but also to increase awareness, to address and improve the quality of life for patients with NBPP via traditional and recent technology-assisted modalities. For NBPP patients with extensive or severe nerve palsies, we strongly suggest early referral to an interdisciplinary specialty brachial plexus clinic to avail the patient of the most current treatment paradigms to achieve the optimal outcome.
