For the nurse practitioner or physician assistant seeing the patient with peripheral nerve injury or disorder, we suggest you include considerations of the following in your initial evaluation, conservative management, and/or referral to a Specialty Center. The initial evaluation of the adult with suspected peripheral nerve involvement includes a thorough History and Physical examination to:
- Establish the diagnosis of Peripheral Nerve Injury or Disorder
- Evaluate for and treat associated conditions including musculoskeletal injuries such as fractures, or other organ injury.
Early education and open communication with the patient and their family can improve the outcomes for peripheral nerve injury patients.
History (HPI)
The history suggested below assesses for parameters that may be associated with peripheral nerve palsy/injury.
Patient’s History
- Onset of symptoms (neurologic deficit/pain)
- Location (upper extremity/lower extremity side)
- Duration (how long has the patient experienced the symptoms and was it immediate after injury; symptoms improving or worsening?)
- Character
- Aggravated by
- Relieved by
- Frequency of occurrence
- Severity of Symptoms
Examination
The examination suggested below can supplement the standard examination.
Observation
Spontaneous movement of arm at:
- Shoulder
- Elbow
- Wrist
- Fingers
- Thumb
Spontaneous movement of the leg at:
- Hip
- Knee
- Ankle
- Toes
Motor Function
Passive Movement
- Clicking or resistance when arm moved by examiner
- Full or decreased range of motion when arm moved by examiner
- Shoulder
- Elbow
- Wrist
- Fingers
- Thumb
- Hip/leg/foot
- Clicking or resistance when leg moved by examiner
- Full or decreased range of motion when leg moved by examiner
- Full or decreased range of motion of the
- Hip
- Knee
- Ankle
- Toes
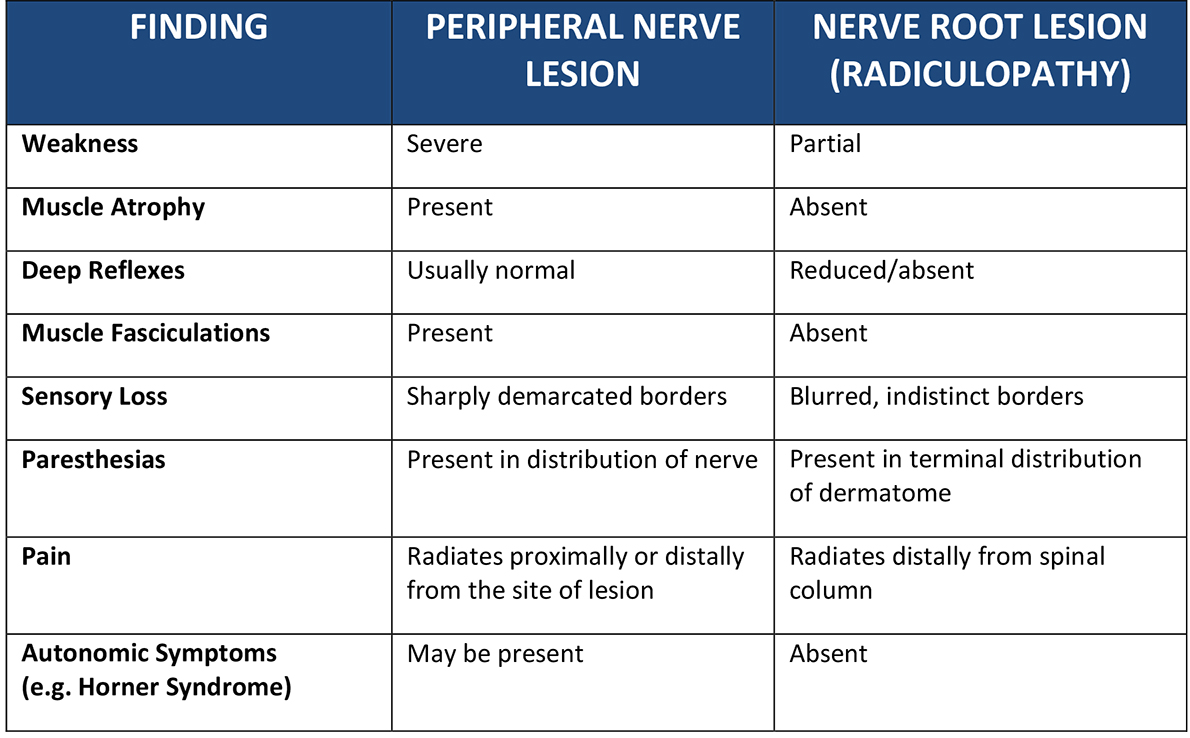 Guide to help clinician differentiate between peripheral nerve lesion and nerve root lesion coming from the spine nerve root lesions (radiculopathy).
Guide to help clinician differentiate between peripheral nerve lesion and nerve root lesion coming from the spine nerve root lesions (radiculopathy). Active Movement
Manual motor testing of individual muscles should be performed using the following grading scale
- 0/5 no contraction;
- 1/5 flicker or trace of contraction;
- 2/5 active movement through full available joint range of motion with gravity eliminated;
- 3/5 active movement through full available joint range of motion against gravity;
- 4/5 active movement against gravity and resistance;
- 5/5 normal power
The movement or activation of the muscle should first be evaluated without resistance. If the patient is unable to perform the movement against gravity, they should be placed in a gravity eliminated position. If full range of motion against gravity is present, the muscle should then be tested against active resistance provided by the examiner.
Upper extremity:
- Trapezius (Spinal Accessory nerve) – shoulder shrug
- Deltoid (Axillary nerve) – shoulder and arm abduction
- Teres Minor (Axillary nerve) – shoulder external rotation
- Infraspinatus (Suprascapular nerve) – shoulder external rotation
- Supraspinatus (Suprascapular nerve) – shoulder abduction above 45o
- Pectoralis Major and Minor (Medial & Lateral Pectoral nerve) – arm adduction and shoulder internal rotation
- Latissimus Dorsi (Thoracodorsal nerve) – shoulder internal rotation, extension and spine extension. Can be tested by asking patient to cough, with the clinician palpating contraction/movement at the posterior axillary fold and border
- Biceps (Musculocutaneous nerve) – forearm flexion and supination
- Triceps (Radial nerve) – elbow extension;
- Extensor Carpi Radialis Longus (Radial Nerve) - extension and abduction of the hand at the wrist;
- Brachioradialis (Radial Nerve) - forearm flexion in neutral position (between supination and pronation);
- Supinator (Radial Nerve) – forearm supination with the elbow fully extended;
- Abductor Pollicis Longus (Posterior Interosseous Nerve) - abduction of the thumb at the carpo-metacarpal joint at a right angle to the palm;
- Pronator Teres (Median Nerve) – pronation of forearm;
- Flexor Carpi Radialis (Median Nerve) – flexion and abduction the hand at the wrist;
- Abductor Pollicis Brevis (Median Nerve) – abduction of the thumb at right angles to the palm;
- Opponens Pollicis (Median Nerve) – touching the base of the little finger with the thumb across the palm;
- Flexor Carpi Ulnaris (Ulnar Nerve) – flexion and adduction of the hand at the wrist;
- Abductor Digiti Minimi (Ulnar Nerve) – abduction of the little finger (5th digit);
- First Dorsal Interosseous Muscle (Ulnar Nerve) – abduction of the index finger;
- Adductor Pollicis (Ulnar Nerve) – adduction of the thumb at right angles to the palm;
Lower extremity:
- Quadriceps Femoris (Femoral nerve) – knee extension and flexion of the hip with the knee flexed;
- Hamstring Muscles (Sciatic nerve) – knee flexion and extension of the hip;
- Gluteus Medius (Inferior Gluteal nerve) – hip abduction;
- Adductor Longus, Magnus and Brevis (Obturator nerve) – hip adduction;
- Gastrocnemius (Tibial nerve) – ankle plantarflexion with the patient supine and knee extended;
- Soleus (Tibial nerve) – ankle plantarflexion with the patient supine and knee flexed;
- Tibialis Posterior (Tibial nerve) – inversion of the foot & ankle;
- Tibialis Anterior (Deep Peroneal nerve) – dorsiflexion of the foot & ankle;
- Extensor Digitorum Longus (Deep Peroneal Nerve) – dorsiflexion of the toes;
- Extensor Hallucis Longus (Deep Peroneal Nerve) – dorsiflexion of the great toe;
- Peroneus Longus and Brevis (Superficial Peroneal Nerve) – eversion of the foot & ankle
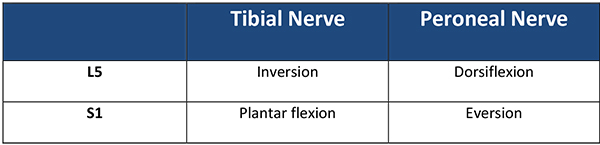 Ankle movements by nerve root guide to help clinician differentiate between a L5 /S1 radiculopathy and peripheral neuropathy.
Ankle movements by nerve root guide to help clinician differentiate between a L5 /S1 radiculopathy and peripheral neuropathy.Sensation - specific outline of dermatomal sensory loss; patient will be able to outline the area of sensory deficits that fits with the specific peripheral nerve injury.
Pain – evaluation of onset, location and extent of pain is critical. Evaluation of current medication, and past medication used for pain management is essential in planning a pain regiment with patient.
Ancillary Testing
Radiographic imaging (MRI, CT, CT myelogram, Ultrasound) can be useful to assess the extent and severity of Peripheral Nerve Palsy/Injury, best performed at a specialty center due to the complexity of the study. X-rays may be useful if skeletal fractures are suspected. Electrodiagnostic (EDX, NCV, EMG) testing is a very specialized study, best performed at a specialty center with an experienced electrodiagnostician. Many published reports indicate that EDX may be overly optimistic, so the EDX must be taken in the context of the clinical history and examination. Interpretation of the EDX findings are quite difficult, and use of the EDX to determine prognosis remains controversial.
The Next Step
Early referral (as soon after injury as possible) of adults with suspected peripheral nerve injury or disorders to interdisciplinary specialty clinics can improve overall functional outcome, regardless of future plans for conservative or surgical management. Occupational /physical therapy (OT/PT) referral should be provided to encourage retention of full range of motion at all joints and to reduce the risk of contractures. Bracing or splint may also be provided to help maintain movement or protect weak joints. Regardless of the extent and severity of the peripheral nerve injury or disorder, OT/PT should be started as soon as possible, except in the presence of skeletal fractures. A home exercise program is critical to increase the likelihood of functional improvement with or without surgical intervention and should be instituted with guidance from OT/PT. For those patients who do not demonstrate progressive substantial recovery by 3 to 6 months after injury, surgical intervention may be helpful to improve functional outcomes of the patient. Options for surgical interventions may include nerve reconstruction, tendon transfers, and skeletal stabilization. If you would like to refer your patient to our specialty center, please click here.
