As your caregivers, we understand that you may have anxiety concerning your diagnosis and that you may feel quite overwhelmed. Becoming more informed about your diagnosis will enable you to cope and better understand your treatment expectations and outcomes. The following information is to help you better understand peripheral nerve conditions and your treatment options.
Anatomy of the Peripheral Nervous System
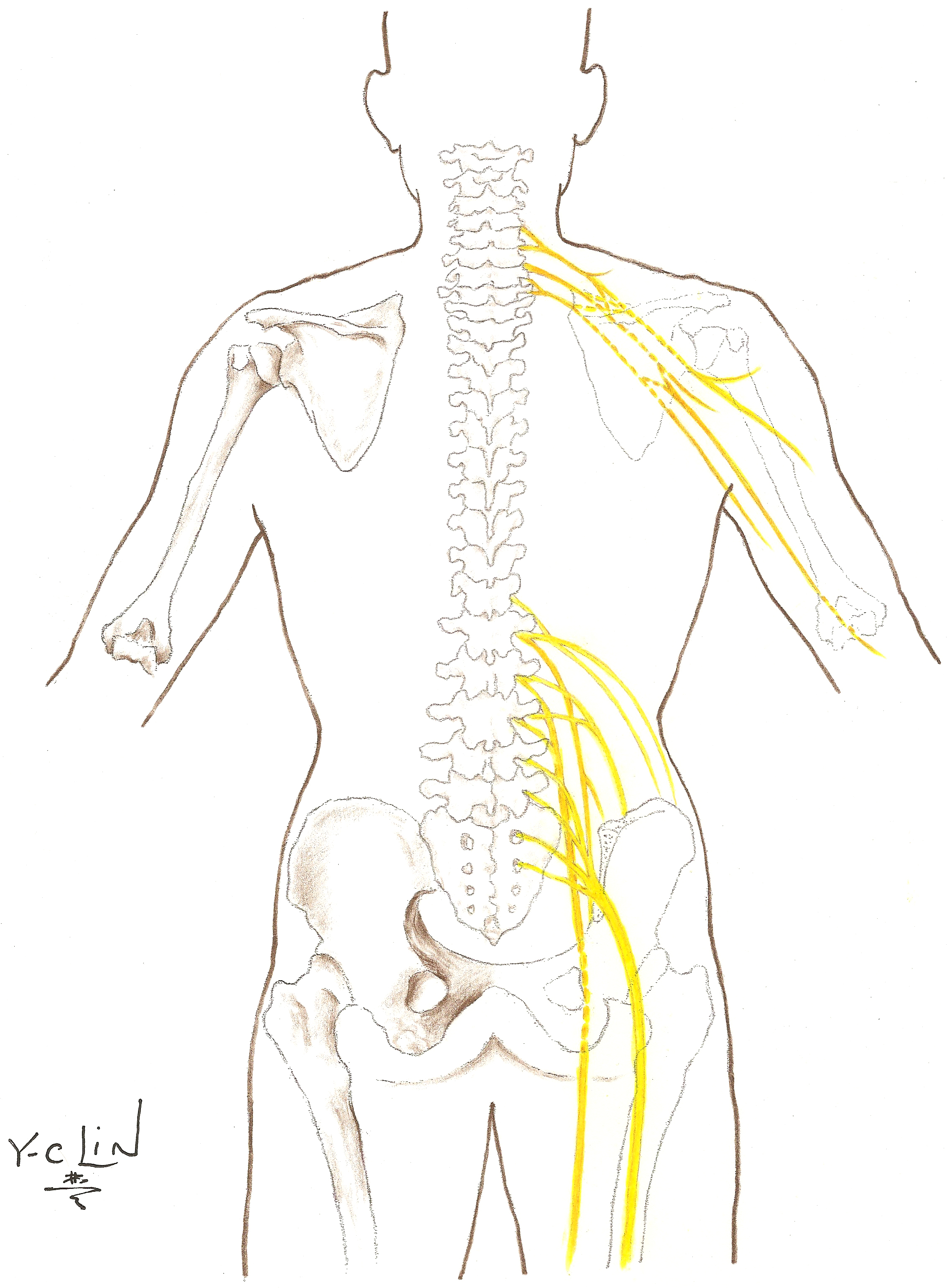
The nervous system is the controlling and communicating system of the body. It includes two major structural systems:
- Central nervous system that involves the brain and spinal cord
- Peripheral nervous system that is made up of nerves extending out from the brain and spinal cord
Peripheral nerves are composed of fibers from many spinal nerves. Most peripheral nerve injuries occur in the arm or the leg.
Brachial Plexus Palsy
Anatomy of the Brachial Plexus
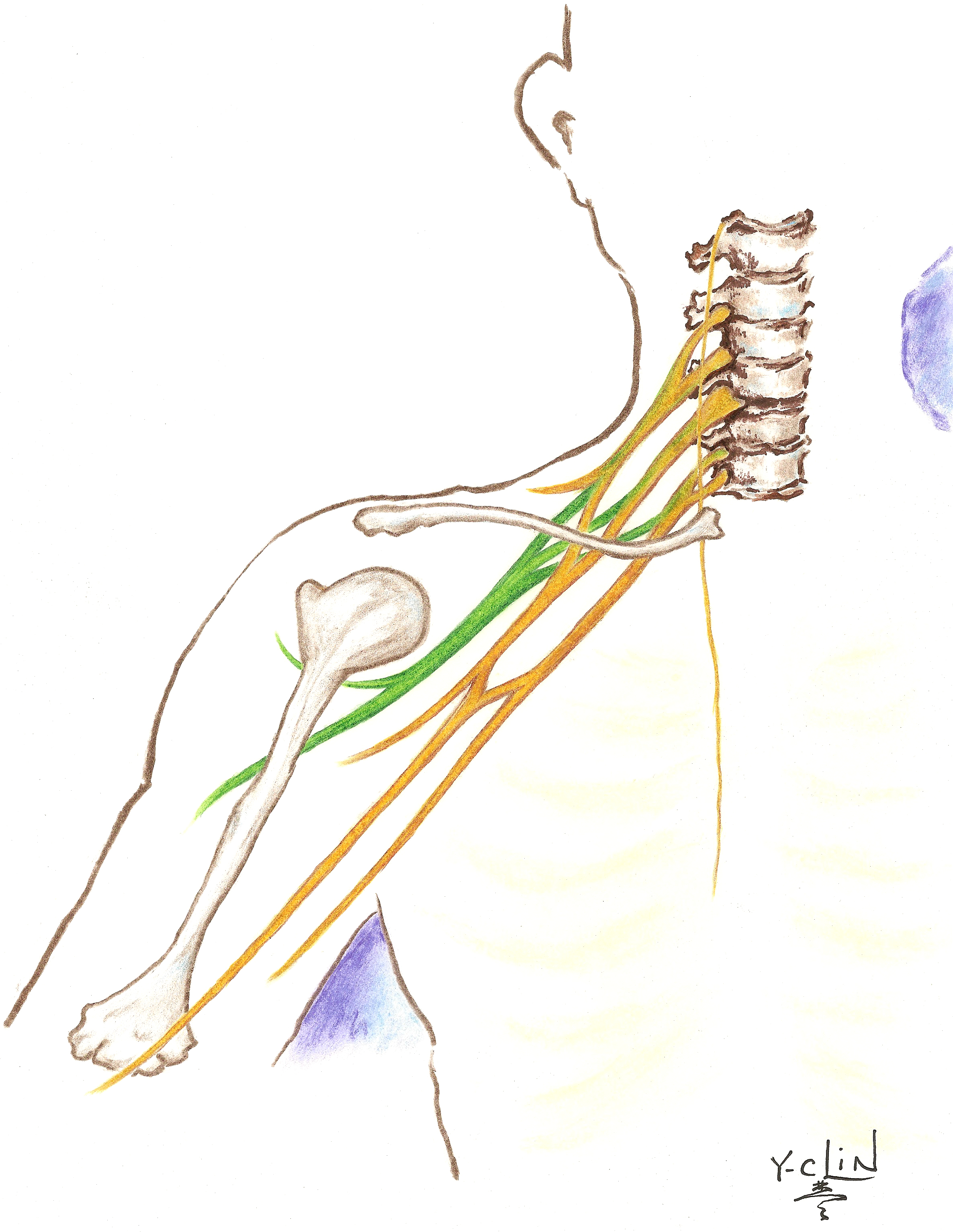
The brachial plexus starts with a collection of five nerve roots: (C5 to T1) that extend from the spinal cord in the neck and run laterally (away from the midline) and inferiorly (toward the feet) to innervate (power) the upper extremity. The brachial plexus supplies all the information for the arm to move and feel.
Injury to the Brachial Plexus
Traumatic injury to the brachial plexus may occur in one or more locations. The nerves may become detached from the spinal cord, or they can become severed remotely from the spinal cord. They can also be stretched or bruised.
Management of Brachial Plexus Palsies
The type of treatment recommended depends in part upon the type of injury that has been sustained.
Conservative management
Occupational therapy (OT) and Physical therapy (PT) are primary treatment recommendations. The goal of therapy is to improve or maintain range of motion, gain strength in the arm, and address factors involving the ability to perform everyday activities.
Surgical management
Several options exist for surgical reconstruction of the brachial plexus. Surgery may include exploration of the brachial plexus, exploration with nerve repair using graft material, exploration with coaptation (connecting two nerves end to end), or exploration with nerve transfer (using a functional nerve to help power one that does not work). Surgery may also include muscle and tendon transfers.
Median Neuropathy
Anatomy of the Median Nerve
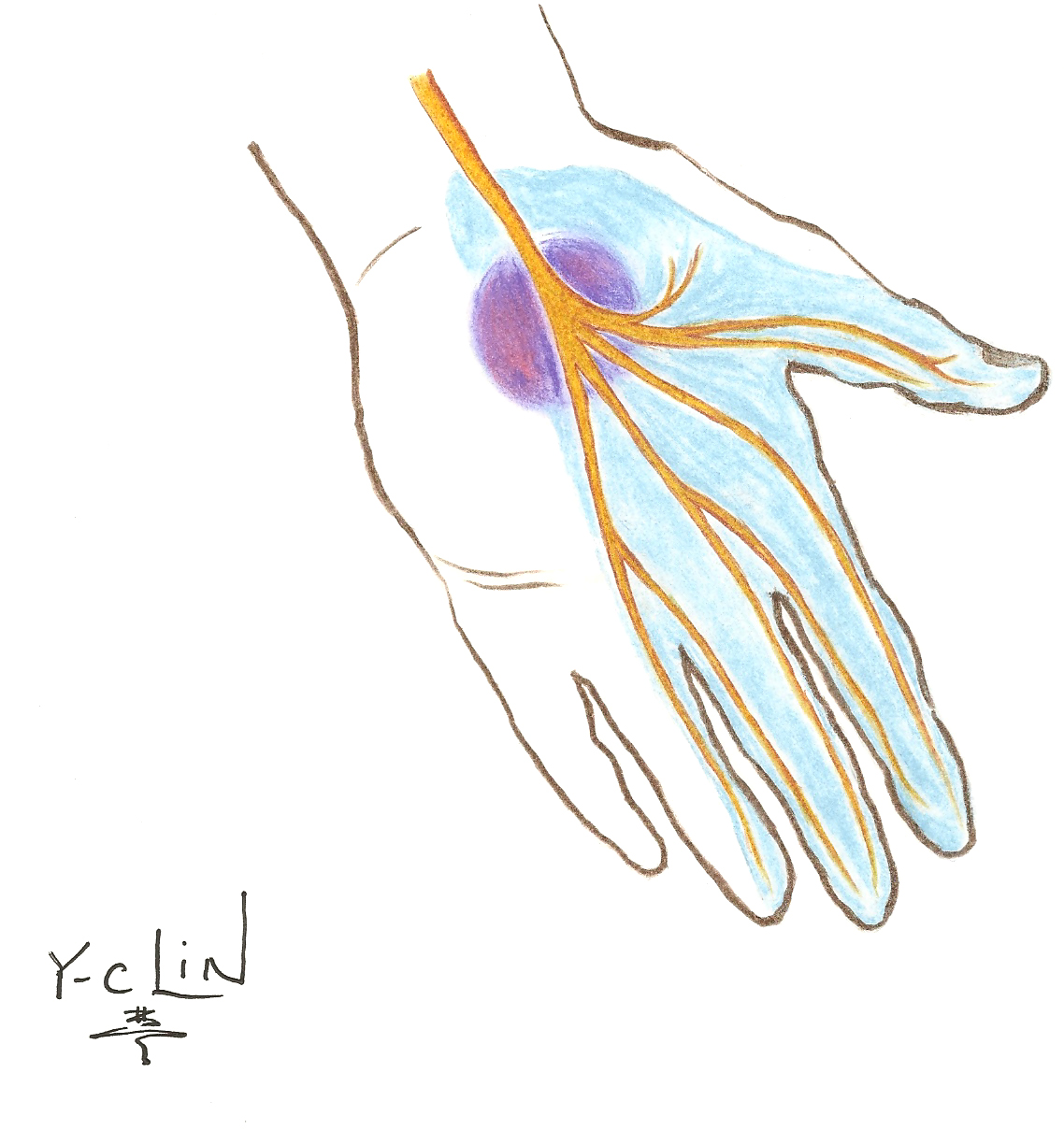
The median nerve originates from the brachial plexus. This nerve provides movement to your forearm and hand and sensation to the hand and fingers. The median nerve is the only nerve that passes through the carpal tunnel. If it is compressed, carpal tunnel syndrome may occur.
Median Neuropathy (Carpal Tunnel Syndrome)
Median neuropathy at the wrist, (carpal tunnel syndrome), is a medical condition resulting from compression of the median nerve. Pressure may be caused by swelling, associated with arthritis, diabetes, or hypothyroidism. Carpal tunnel syndrome may also occur during pregnancy. Symptoms may include: pain, numbness, or tingling in your hand and wrist, particularly in the thumb and middle fingers, which may radiate up into the forearm. Pain increases with the use of your hand. For example, pain may increase when you are driving or reading and it may also intensify during the night and when you first awake. Eventually muscle deterioration can develop in the thumb.
Management of Carpal Tunnel Syndrome
Conservative management
Splinting the wrist during sleep and during physical activity may decrease pain. Occupational/Physical therapy may also reduce your symptoms. Steroid injections can similarly be effective.
Surgical management
If your symptoms do not respond to conservative treatment, surgery may be a reasonable option for relief of symptoms. Surgery may halt the progression of symptoms and prevent further loss of function.
Ulnar Neuropathy
Anatomy of the Ulnar Nerve

The ulnar nerve controls most of the fine motor movement of the hand and sensation to the little finger and half of the ring finger. The ulnar nerve runs near the ulna bone in the arm and is located at the distal (far end) of the humerus near the elbow. It is sometimes referred to as the “funny bone,” as striking this nerve can cause a tingling sensation and pain.
Ulnar Nerve Injury (Ulnar Neuropathy)
Ulnar neuropathy can result from entrapment or compression of the ulnar nerve. This condition can result in numbness, tingling and/or pain to the arm and hand on the side of the little finger and half of your ring finger.
Management of Ulnar Neuropathy
Conservative management
Elbow padding or splints to keep the arm straight may reduce discomfort. A home exercise program may also be beneficial, as it can show you ways to reduce and prevent discomfort.
Surgical management
Surgery may be recommended if conservative treatment does not relieve your symptoms or if you are losing function in the affected hand. Early diagnosis of ulnar neuropathy may prevent progression of your symptoms and avoid loss of function.
Lower Extremity Nerve Injuries
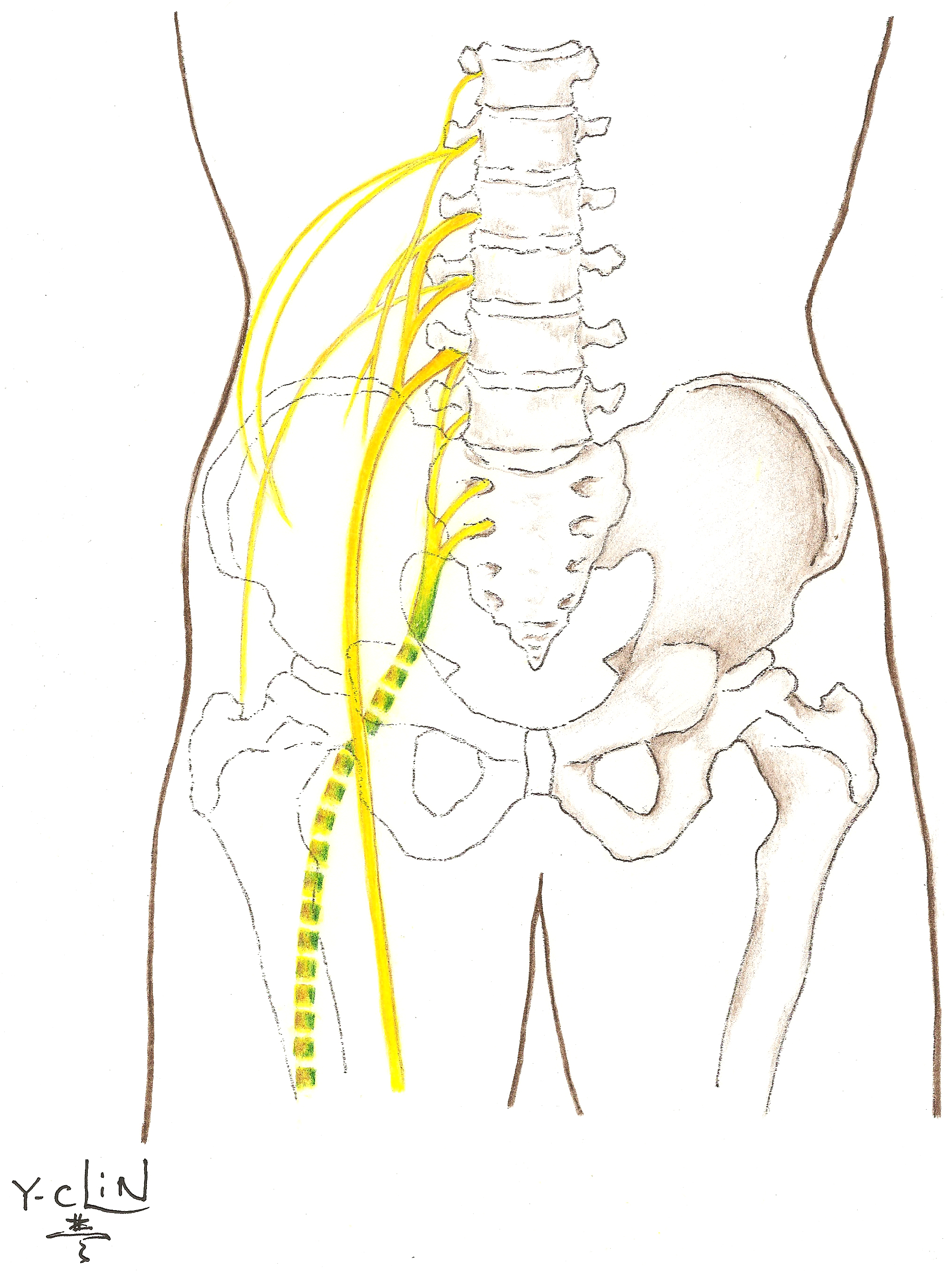
The nerves controlling lower extremity function originate in the low back (lumbosacral area). As the nerve roots leave the spinal cord, they form a network or plexus that quickly divides into distinct nerves. The most commonly affected nerve of the lower extremity is the sciatic nerve and its branches that run through the buttocks and down the back of the leg. The sciatic nerve then divides into the peroneal nerve and the tibial nerve near the knee:
- The peroneal nerve allows you to point your foot up and turn it outward.
- The tibial nerve allows you to stand on your toes.
Sensory branches affected in the lumbar plexus:
- Iliohypogastric nerve is the sensory branch leading to the skin of the lateral hip.
- Ilioinguinal nerve is the sensory branch that passes through the external inguinal ring to the skin over the pubic symphysis and lateral aspect of the labia majora or scrotum.
- Genitofemoral nerve splits off into two sections, supplying sensation to the upper inner thigh and genital regions:
- Femoral branch innervates the skin below the inguinal ligament/groin area
- Genital branch innervates the male scrotal skin or female labia majora
- Lateral femoral cutaneous nerve supplies the skin with sensation on the anterolateral part of the thigh.
Peroneal Neuropathy
Anatomy of the Peroneal Nerve
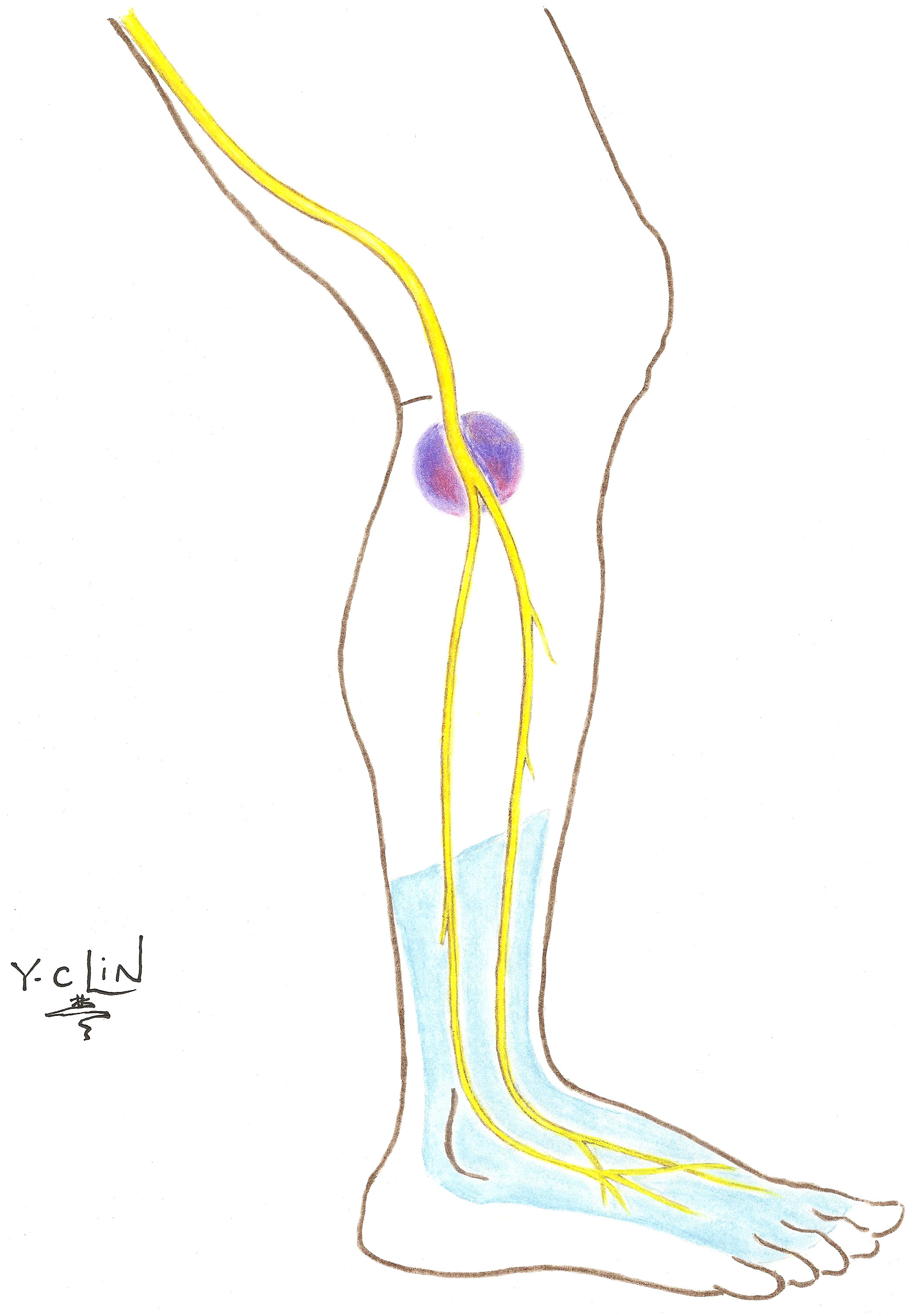
The peroneal nerve originates from the sciatic nerve and innervates the calf and the foot. It passes around the neck of the fibula (the smaller of the lower leg bones) then passes toward the front through an opening near the attachment of the long peroneal muscle group, where it divides into two branches: the superficial peroneal and the deep peroneal nerves.
Peroneal Neuropathy
The peroneal nerve is frequently subjected to trauma secondary to its superficial location, and injury of this nerve can occur with high impact trauma to the legs. Damage to the peroneal nerve can result in a foot-drop or toe drop and inability to evert the foot. With such an injury, walking can be difficult without brace support.
Management of Peroneal Neuropathy
Conservative management
An orthotic may be necessary to hold the foot in a neutral position during the recovery phase. It can provide support while walking until the nerve recovers.
Surgical management
Surgical intervention may be recommended if symptoms do not improve with conservative treatment. Surgery may be indicated when a tumor is compressing the nerve, the nerve is being compressed by tendons or muscle, or there has been a cut to the peroneal nerve.
Nerve Sheath Tumors
Neuromas
Note that a neuroma is a non-cancerous (benign) growth of nerve tissue that can develop in various parts of your body in response to injury. It is not actually a tumor. Rather, it is a normal physiologic response by an injured nerve. Injury may cause the nerve to swell and regenerate that can cause symptoms such as tingling, burning, numbness and /or pain. Anything that causes compression or irritation of the nerve can lead to the development of a neuroma.
Types of Peripheral Nerve Tumors
Schwannoma
A schwannoma is a benign neoplasm thought to originate from Schwann cells located in the myelin sheath covering axons. The tumor is typically encapsulated and usually found on the outside of the nerve. Schwannomas are benign, but must be distinguished from neurofibroma and Malignant Peripheral Nerve Sheath Tumor (MPNST). Schwannomas may cause symptoms similar to other tumors. The symptoms include: numbness, tingling, pain, or motor weakness.
Neurofibroma
A neurofibroma is a benign nerve tumor. Neurofibromas may be harmless or may cause serious damage by compressing nerves and other tissues or organs. The tumors may cause bumps under the skin, colored spots, skeletal problems, pressure on spinal nerve roots or other neurological problems.
Malignant peripheral nerve sheath tumor
Malignant peripheral nerve sheath tumors tend to arise along nerves, usually affecting arms or legs. They can also arise in the abdomen or head and neck region. In rare cases, they can spread to local lymph nodes or lungs. This tumor can be associated with a condition called neurofibromatosis. Symptoms depend on the primary site of disease, but they often appear as an enlarged mass that can be associated with pain or changes in sensation, eventually resulting in severely debilitating neurologic deficits. This tumor is rare.
Management of Tumors
Treatment depends on the type and location of the nerve tumor.
- If you have a benign tumor and no neurologic deficits, recommendations are usually conservative.
- If the tumor is causing neurologic deficits or if malignancy is suspected, the recommendation is to resect the tumor. At time of excision, a pathologist will review a sample of the tumor to determine the diagnosis.
- In the most severe type of malignant tumor, a wide resection or amputation may be recommended, along with radiation and chemotherapy.
What to Expect at Your Clinical Evaluation
- The nurse practitioner will obtain your medical history and physical exam.
- You may be evaluated by other members of the team.
- An electrodiagnostic (EDX) study may be recommended. EDX studies provide us with information about the location and severity of the injury, along with any recovery of nerve function. Electricity is the means of communication by the nervous system, and both motor and sensory function depends upon good electrical conduction. This test may be completed by one of our electrodiagnosticians prior to your visit with us.
- You may undergo radiological studies. Radiologic studies using computer tomography (CT), ultrasound (US), magnetic resonance imaging (MRI), or CT myelogram assist in diagnosing your condition. These studies can be used to assess for avulsed nerves (nerves that have become detached from the spinal cord).
- Results. The results of your medical history and physical examination will be communicated to one (or more) of our surgeons or physicians. After comprehensive evaluation, the physicians(s) will discuss their findings and make treatment recommendations.
