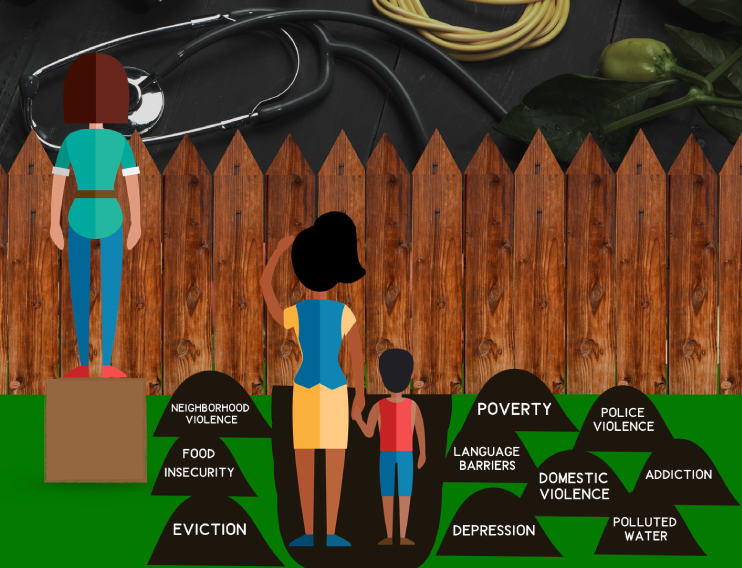
 Social Determinants of Health Graphic by Christina Czuhajewski, Creative Commons License BY-NC-SA
Social Determinants of Health Graphic by Christina Czuhajewski, Creative Commons License BY-NC-SA
Primary care physicians know that a whole world of social factors influence their patients' ability to manage their chronic diseases. Conversations with patients about their self-care often touch on the underlying financial, social, and environmental variables--also referred to as social determinants of health--that encourage or discourage healthy behaviors associated with disease prevention and management. In these conversations, a patient's full health "story" may emerge, full of rich, contextual information that can be leveraged for improved care. A new study that draws on qualitative interviews with primary care physicians, finds that electronic health record (EHR) systems may not have the capacity to use the underlying psychosocial information that emerge in clinical encounters.

The study was led by Rutgers University School of Communications and Information Assistant Professor Charles Senteio, Ph.D., M.B.A., M.S.W., during his time as a Ph.D. candidate at the University of Michigan School of Information. With support from his dissertation research committee, including Caroline Richardson, M.D., the Dr. Max and Buena Lichter Research Professor of Family Medicine, Senteio and his colleagues identify opportunities to improve EHR capabilities and work flow process to improve the collection and use of this type of patient information. The study is the first of its kind to describe physicians’ perspectives on how EHR adoption has impacted their ability to collect and use information that helps tell the patients’ story.
The paper was published in the May 2018 International Journal of Medical Informatics, and is entitled, Physicians’ Perceptions of the Impact of the EHR on the Collection and Retrieval of Psychosocial Information in Outpatient Diabetes Care.” Fellow dissertation committee members and co-authors also include Tiffany Veinot, Ph.D, Julia Adler-Milstein, Ph.D., faculty members at the University of Michigan School of Information.
Read More: Dr. Richardson receives distinguished research mentor award
“The central point of the paper,” Senteio said, “is to highlight where capabilities need to be improved.”
Describing how their work compares to similar research in the health informatics field, he said, “We are not aware of another study that investigates providers’ perceptions of how EHR adoption has influenced the capture and use of psychosocial information to make clinical decisions for outpatient diabetes care. This is an important research topic, because, even with the wide-scale adoption of EHRs that help support clinical decisions, chronic disease disparities persist. And these disparities are, in part, driven by psychosocial factors, like financial strain and level of social support.
“Other studies have described how EHRs are not particularly adept at capturing psychosocial information. The novelty of this study lies in that we actually went to practitioners with experience with outpatient diabetes care to get their perspectives.”
Explaining how this paper will directly help improve EHR capabilities to enhance patient care, Senteio said, “We all have ‘self-care’ which for chronic conditions like diabetes basically boils down to four ‘behaviors’: 1) medication behavior, 2) dietary behavior, 3) attendance at follow-up appointments, and 4) physical activities. But few of us consistently have behaviors that align with recommended self-care (or sometimes called self-management). This study will help inform developers to direct enhancement to EHR capabilities to include the capture and use of psychosocial information, which include aspects of social determinants of health.”
Asked if doctors find current EHRs limiting and difficult to work with, Senteio said, “Well any clinician I’ve talked to is already well aware of EHR limitations! But while we continue to investigate the impact that environment and ‘lived experience’ has on health behavior, we must also understand what tools practitioners have in their attempts to support patients in these decisions. In addition to informing development of EHR capabilities by understanding our ‘systems’ limitations, I think it is important to illuminate the important role that psychosocial factors have in healthcare. I think this awareness can help spur increased practitioner-patient engagement. After all, if a ‘system’ requires that a practitioner inquire about financial strain, then that might prompt practitioners to engage differently with their patients, and vice versa.”
The paper concludes with the recommendation that EHR tools and workflows should be re-designed. Asked what ideal workflows and EHRs might look like, and how much he thinks they could improve outcomes for diabetes patients, Senteio said, “I don’t have enough background in clinical operations to state what ideal workflows would look like, but I can comfortably assert that closer to ideal would involve health information exchange for elements necessary for equitable care, and there is no quality care without equitable care. Period. This health information exchange should include psychosocial information like poverty, level of social support, and exposure to violence - including domestic violence.
“Obviously these factors are not at play equally for every patient, at every visit, but our workflows should enable this type of information exchange if pertinent, which of course include the practitioner-provider relationships necessary to facilitate this exchange. Also, I think allied health professionals are critical to help transform our system of care. For example, community health workers, nurses, and social workers are critical parts of any ambulatory care team concerned with providing quality care, which of course means equitable care. Last, ideal clinical workflow will be informed by a wonderful quote written over 100 years ago by Sir William Osler, the father of modern medical education: “Ask not what disease the person has, ask what person the disease has.”
Read the original press release from the Rutgers School of Communications and Information
Article Citation: Senteio C, Veinot T, Adler-Milstein J, Richardson CR. Physicians’ perceptions of the impact of the EHR on the collection and retrieval of psychosocial information in outpatient diabetes care. International Journal of Medical Informatics. 2018;113:9-16. doi:10.1016/j.ijmedinf.2018.02.003.
Browse the latest research in clinical informatics and technology and preventive medicine from the Department of Family Medicine.


