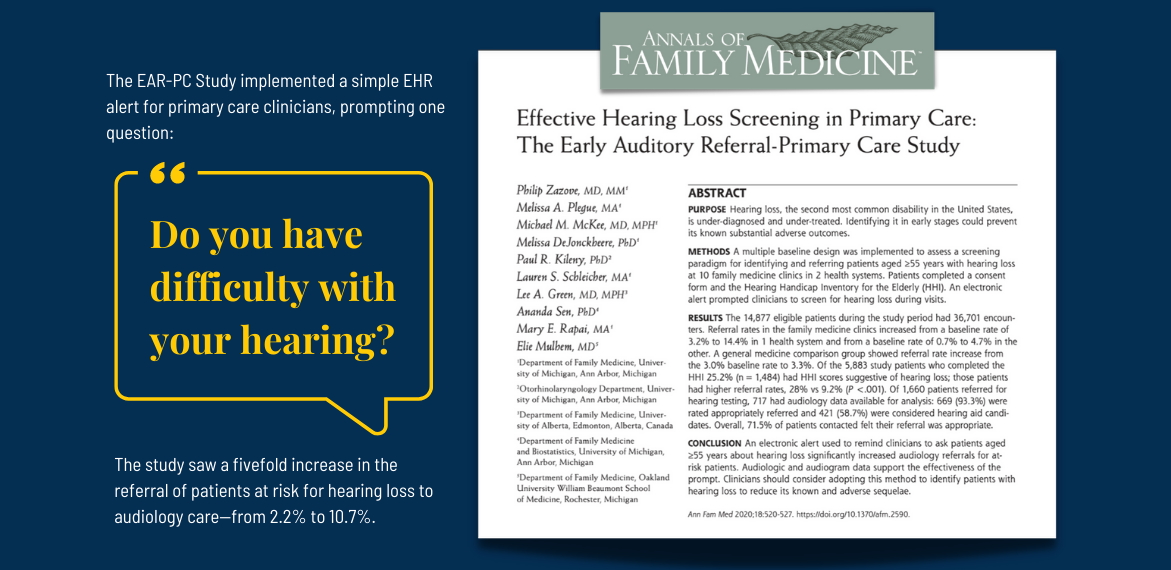
An electronic health record alert that reminded primary care clinicians to ask patients aged older than 55 years about their hearing significantly increased the number referrals to an audiologist, according to new findings published in the Annals of Family Medicine.
Hearing loss is the second most common disability in the United States and comes with it a higher risk for being diagnosed with significant health conditions, such as hypertension, diabetes, dementia and depression, as well as higher health care cost and use. The Early Auditory Referral-Primary Care (EAR-PC) study was designed to address the lack of data about hearing loss screening.
READ ALSO: Hearing aids linked to lower risk of dementia, depression and falls
The EAR-PC study is led by Philip Zazove, M.D., professor and the George A. Dean, M.D., Chair of Family Medicine. The study team includes several U-M Family Medicine faculty and staff including Melissa A. Plegue, biostatistician; Michael M. McKee, M.D., M.P.H., Associate Professor; Melissa DeJonckheere, Ph.D., Assistant Professor; Lauren S. Schleicher, M.P.H, and Mary E. Rapai, research coordinators; Ananda Sen, Ph.D., the Lee A Green Collegiate Research Professor; Lee A. Green, M.D., M.P.H., Professor Emeritus; as well as Paul R. Kileny, Ph.D., Professor in the Department of Otolaryngology-Head and Neck Surgery at the University of Michigan; and Elie Mulhem, M.D., of Beaumont Health.
Zazove and colleagues asked older patients (n = 14,877) at two Michigan health systems to complete the Hearing Handicap Inventory (HHI) before their appointments. Most of the patients were female and white. Faculty, residents and midlevel clinicians who did not have access to the patients’ HHI results received an EHR alert during the appointments, prompting them to ask: “Do you have difficulty with your hearing?”
The study, which lasted 31 months, showed that audiologist referrals increased from 2.2% to 10.7%. Specifically, the audiologist referral rates at one health system increased from 3.2% at baseline to 14.4%, and from 0.7% to 4.7% at the other system. Among a comparison group of patients aged 65 years and older who attended annual wellness visits, referrals increased from 3% to 3.3%.
Among 5,883 patients who completed the HHI, approximately one-quarter had scores suggestive of hearing loss. According to the researchers, 28% of patients with positive HHI scores were referred based on the screening question compared with only 9.2% of those with negative HHI scores.
“The 72% of participants with a positive HHI who were not referred is likely due to a combination of patients not admitting their hearing loss, clinicians too busy to address the alert and patients declining referrals,” Zazove and colleagues wrote in the Annals of Family Medicine. “Of note, our population hearing loss rates (using HHI data) were similar to other studies, suggesting that our outcomes are applicable to typical community populations.”
Also, among 717 of 1,660 patients referred to audiologists, 93.3% were “appropriately referred,” 85% had hearing loss (mostly mild) and 58.7% were considered candidates for hearing aids.
Researchers concluded the EHR alert helps “increase the chances that hearing loss patients ... will get better and earlier hearing health care with potentially fewer hospitalizations and improved quality of life.”
Article Citation: Zazove P, Plegue MA, McKee MM, et al. Effective Hearing Loss Screening in Primary Care: The Early Auditory Referral-Primary Care Study. The Annals of Family Medicine. 2020;18(6):520-527. doi: 10.1370/afm.2590.