Showing 1-15 of 20 results
Health Lab
At-home test can detect tumor DNA fragments in urine samples, providing a non-invasive alternative to traditional blood-based biomarker tests

Department News
Meet the newest residents to join our program

Health Lab
2 in 3 parents in national poll say their child ages 5-12 use personal audio devices; pediatrician offers 4 tips to reduce noise exposure risks

Health Lab
Elective surgery study shows older adults have concerns about what it will cost them, how much work they’ll miss and whether they’ll catch COVID-19.

Health Lab
With over 400 stories published on Health Lab in 2023, the following 10 articles were the most read of the year.
Health Lab
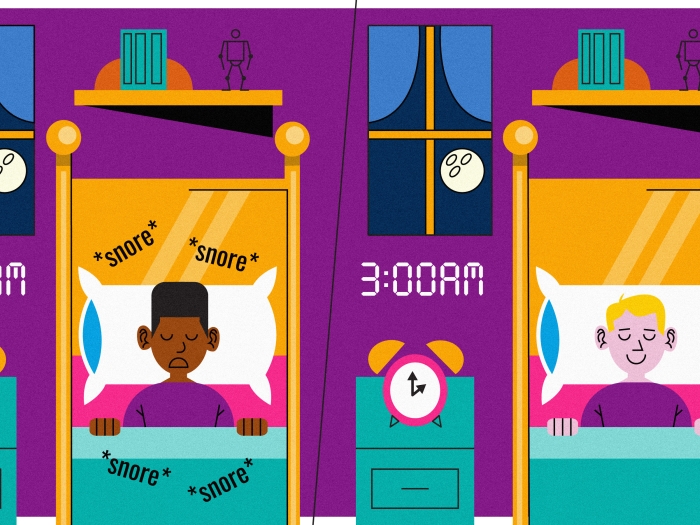
As researchers explored potential reasons behind racial disparities in treatment outcomes for children with severe sleep apnea, they were expecting to find the answer in socioeconomic factors. But they were surprised to learn that when one risk factor – obesity – was taken out of the equation, race was no longer associated with worse post-surgery outcomes for obstructive sleep apnea.
Department News
Congratulations to Gifty Kwakye, MD, MPH, and Andrew G. Shuman, MD, FACS, HEC-C, on their new roles.

Department News
U.S. News and World Report annually evaluates hospitals for its Best Hospitals list by evaluating data from 4,500 hospitals on a range of criteria, including patient experience, outcomes, care-related factors, and expert opinions from physician surveys.

News Release
There are 13 U-M graduate medical education programs ranked in the top 10 by Doximity.

Health Lab
Tinnitus, the ringing, buzzing or hissing sound of silence, impacts 15% of adults in the United States have tinnitus. A recent study from researchers at the University of Michigan’s Kresge Hearing Research Institute suggests relief may be possible with treatment.

Department News
The management of voice and breathing disorders is a subspecialty of speech-language pathology (SLP).

Health Lab
The University of Michigan Health System received an order for a cervical orthosis, or neck brace, which resulted in a modified version still being used today, changing recovery for the better.

Health Lab
New effort responds to concerns about opioid overdose, misuse and side effects in kids; Expert shares 8 things parents and pediatric surgeons should know

Health Lab
Audiologists can help with more than your hearing; they can also help with better speech and balance for children and adults.