The last six months of my family’s life have been hell.
But our teen daughter was suffering silently long before that, as an eating disorder took over her mind and body.
My husband and I just didn’t know it.
Today, after a heart-wrenching journey for all of us, she’s on the road to recovery. As I look back, I realize how many warning signs we missed. I see how little awareness most parents have of what to look for, how dangerous eating disorders are, and how hard the journey to recovery can be.
That’s why I’m sharing our story, though without our identity attached because of the stigma that these diseases still carry.
Welcome to Eating Disorders World
Six months ago, our daughter revealed she had been making herself throw up for months, that she never ate at school, and that she tried to “cancel out” the calories she had eaten by exercising.
An eating disorder had taken control of her mind, convincing her she was unworthy of happiness, friends or love; that she should hide from public view; and that nothing mattered except the shape and weight of her body. She had felt this way for years.
She literally wanted to die because a voice inside her head told her she was “fat.”
But she had gotten so good at hiding all of this that we just thought she was having mild depression and got her treatment for that.
Then the truth came pouring out, during a mental health crisis the first week of this school year.
Suddenly, our family found ourselves launched into Eating Disorders World. It’s a topsy-turvy place that thousands of families discover the hard way every year.
“National data demonstrate increased hospitalization rates of adolescents with eating disorders even before the onset of the COVID-19 pandemic. Since then, the rate of teens seeking treatment for eating disorders has dramatically increased, with an even greater demand for already limited access to specialized care,” says Maria Tocco, M.D., a child and adolescent psychiatrist with the Comprehensive Eating Disorders Program at University of Michigan Health C.S. Mott Children's Hospital.
What I wish I’d known about eating disorders
After six excruciating months, we haven’t escaped Eating Disorders World. But our daughter is on the road to recovery, both physically and mentally.
Here are some key things I want to share with parents and guardians who might be as clueless as we were or might suspect something’s not right but can’t put their finger on it.
1. Eating disorders are real mental health conditions, not a matter of control, willpower or bad parenting.
The best comparison I’ve seen, in private online support forums, is that an eating disorder is a terrorist that hijacks your child’s brain.
That terrorist might tell them to stop eating, to exercise compulsively, to avoid all but a few “safe” foods, to make themselves vomit up the food they just ate, to binge on high-calorie food in secret, to despair over their reflection in the mirror or the number on their scale, or to eat only a very low number of calories each day.
Sometimes the voice tells them to hurt themselves if they fail to comply, by cutting or picking their skin, or other “punishments.” It can even suggest they’d be better off dead.
It’s a powerful voice that is impossible to resist without help.
Eating disorders often involve other mental health concerns, such as depression, anxiety or obsessive-compulsive disorder.
In fact, the intertwining of these issues helps make eating disorders so hard to detect and treat – and makes the risk of suicide so high.
2. Eating disorders aren’t caused by any one thing, but many factors can raise risk.
Genetics, stress, personality type, social interactions like teasing and bullying, popular culture and social media can all mix to raise eating disorder risk.
In our daughter’s case, her risk likely arose from a mix of family history of anxiety and larger body sizes, the stress and disruption of the pandemic (including the deaths of several beloved older adults), and the ability to do so much schoolwork and interacting with friends in isolation via screens so she didn’t have to be “seen.”
Other contributors included perfectionist tendencies, weight-related teasing by classmates in elementary school, and the overt and unspoken things she saw on television and social media about which kinds of bodies are attractive, valued and “healthy.”
I wish we had known all of this – especially the genetic risks -- so we could have been on higher alert. Just like other mental health conditions, inherited risks for eating disorders can be triggered by stress and trauma.
I wish we had known about all the places on the web and social media where eating disorder “influencers” show kids tips for restricting their eating and hiding signs of eating disorders or self-harm, or simply show off their starved bodies.
I also wish our society didn’t tolerate shaming and jokes about people with larger bodies in sitcoms, movies, advertisements and viral videos. I’m now far too aware of how pervasive weight-related jokes, memes and trolling are in our culture.
3. Don’t trust stereotypes.
If you had asked me seven months ago what someone with an eating disorder looked like, I would have said a skeleton-thin rich white teen girl.
It’s true that anorexia is more common in teen girls, and some restrict their eating to such an extreme that they take on the stereotypical appearance. However, many other kids and teens can have eating disorders.
“Studies have shown that individuals of any race, body shape, gender identity, and age can develop eating disorders. The stereotypes long associated with eating disorders can lead to costly delays in treatment, often because doctors overlook emerging symptoms due to misconceptions about who is affected by them,” says Tocco.
Another key group is kids and teens who are involved in high intensity sports or dance. In fact, some parents have shared that the emphasis on body weight or appearance in activities -- from wrestling and swimming to ballet and gymnastics -- helped trigger their child’s eating disorder.
And then there are kids like my daughter, whose weight-to-height ratio stays in the normal or high range, even when they’re losing weight by restricting and making themselves throw up. This is sometimes called atypical anorexia and impossible to spot from a person’s outward appearance.
4. The earlier someone gets help the better, so heed warning signs.
Eating disorders may be based in the brain, but they take a terrible toll on the rest of the body. After all, food is fuel, especially in a body that’s still supposed to be growing.
That’s why it’s so important to get children and teens help early, before they suffer long-term physical damage to organs, tissues and metabolism -- and before food-related behaviors get too entrenched.
Lack of nutrients, calories and regular digestion of food can lead to physical symptoms that are hard to pin down.
In our daughter’s case, she’d complained of headaches, weakness, getting tired easily, vague pains and digestive tract issues. But checkups and blood tests didn’t show a cause.
She started doing worse at school, was easily distracted and fell asleep at odd times.
Some parents have said that their warning signs were on the growth chart that their child’s doctor or nurse practitioner uses to track weight and height over time.
Unexplained weight losses or plateaus in a child who should be growing should be red flags. But the pandemic interrupted regular in-person care for many kids, so those growth charts might be incomplete.
Our daughter also sought out super-baggy clothes, wanted to eat meals alone, and asked to drop out of activities or skip events. It’s easy to chalk these up to teen rebellion, changing interests and depression. But they were all key symptoms of not wanting to be “seen” because of how she felt about her body and how she thought it compared to others. They also masked weight loss.
Refusing to go to school, stay in school all day, or to eat at school are other warning signs and can lead to slipping grades. Eating disorders can make a child have constant worries that their classmates are judging their body size harshly. And an undernourished brain can’t focus on classwork and homework.
5. Treatment can help – but it takes both specialized professional care and intensive family support.
Treating eating disorders, and achieving recovery, is a team sport. And it’s a marathon, not a sprint.
“Eating disorders are complex conditions that impact both the physical and mental health of those affected. For this reason, we recommend taking a multidisciplinary approach to treatment,” Tocco says. “This includes talk therapy with a trained mental health professional and nutrition counseling with a specialized dietician. Individuals should also seek medical care from a clinic that has experience monitoring for and treating the physical effects of the illness, such as nutrient deficiencies and heart conditions. Medications like antidepressants, preferably prescribed by an experienced mental health prescriber, may also be helpful.”
And then there’s food. For someone with an eating disorder, food is medicine.
But because it’s also the very thing that they’ve built their lives around avoiding, restricting, bingeing or purging, it’s often the hardest medicine to take.
The recommended “dosage” in the recovery period is three meals and two to three snacks a day, on a regular schedule. The emphasis is on getting enough calories into them that they can regain the lost weight and then some. They also work to overcome fears or self-imposed restrictions about specific foods.
Studies have shown that this is critical to getting back on track with normal growth, metabolism and hunger-related sensations, and overall recovery.
6. Treatment options vary in intensity and availability.
I had no idea before we started this journey just how hard it is to get access to good care for eating disorders.
There are specialized programs around the country, but availability varies widely. Waiting lists are all too common, leaving families trying to cope while awaiting a spot.
If the mental or physical effects of the disorder have gotten bad enough to cause a crisis, the first stop may be the emergency room and then a bed in a psychiatric hospital unit – something that’s in incredibly short supply nationwide.
More stable but seriously ill patients might go to a residential treatment center, for round-the-clock care and supervision that’s cut off almost entirely from the outside world.
We caught our daughter’s disorder early enough that she could start with a less-intense level of care: a ‘partial hospitalization program’ or PHP. The nearest one with an opening was about an hour’s drive from our house – and we are lucky it was that close.
For nearly two months, she spent six hours each weekday in various kinds of talk therapy, nutrition education, mental and physical evaluations, and having supervised breakfast, lunch, snacks and discussions in a group setting with other teens like her.
Strict protocols ensured she ate or drank an adequate number of calories, no matter how long it took. Strict rules about bathroom trips aimed to prevent purging – and we had to follow the same rules at home. But she got to go home each weekday evening, and all weekend, to sleep in her own bed.
She resisted going to PHP mightily many days, because the eating disorder ‘terrorist’ told her she didn’t need it. But once she had made enough progress to get discharged, she began weekly therapy with a psychologist who specializes in eating disorders, plus regular physical monitoring and medication adjustments from Michigan Medicine’s Comprehensive Eating Disorders Program.
Michigan Medicine and other sites offer more intensive outpatient programs as well. And the rapid rise of telehealth during the pandemic has made it possible for some patients to get entirely virtual eating disorder care. This can make a big difference if they don’t live near a center or therapist offering in-person care.
7. The journey is hard on families, but it’s important to stick with it.
In many ways, I feel lucky. We caught our daughter’s problem before it caused serious physical harm. My family is fortunate to have access to specialized services in our area. We have insurance that has covered much of her care -- though we’ve had to apply for reimbursement for out-of-network care when in-network sites were full.
My husband and I also both have reliable cars, work-from-home flexibility, and jobs with paid time off, so we could spend two hours driving to and from the PHP center, and still get some work done from our laptops at a nearby library. These days, we take her to appointments and can stay home with her on days when she still can’t face going to school.
Many families don’t have these advantages. Some parents must take unpaid family medical leave or quit their jobs to take care of a teen with an advanced eating disorder. Which is another reason early detection is crucial.
Even so, this has been an incredibly hard time, disrupting our work lives and our daughter’s education. We’ve cut out almost all outside activities, gatherings and travel.
We’ve also locked up household objects that she could use to harm herself if the terrorist in her head tells her to punish herself for eating.
Which it has tried to do.
The other thing I wish I’d known about was the sense of isolation – the feeling that you can’t tell anyone what’s going on because eating disorders are so misunderstood and stigmatized.
We’ve only confided in a few family members and friends, her school and our work supervisors. I’m so grateful for the community of eating disorder parents that I’ve found online. Without their support and wisdom, and resources from nonprofit organizations like FEAST and the National Eating Disorders Association, I don’t know where we’d be.
This isolation adds to the distress and worry that claws at any parent with a seriously ill child. And we know that we and our daughter may be battling this illness for years to come.
But we love her so much that we’ll do what it takes – including trying to help other families know more than we did.
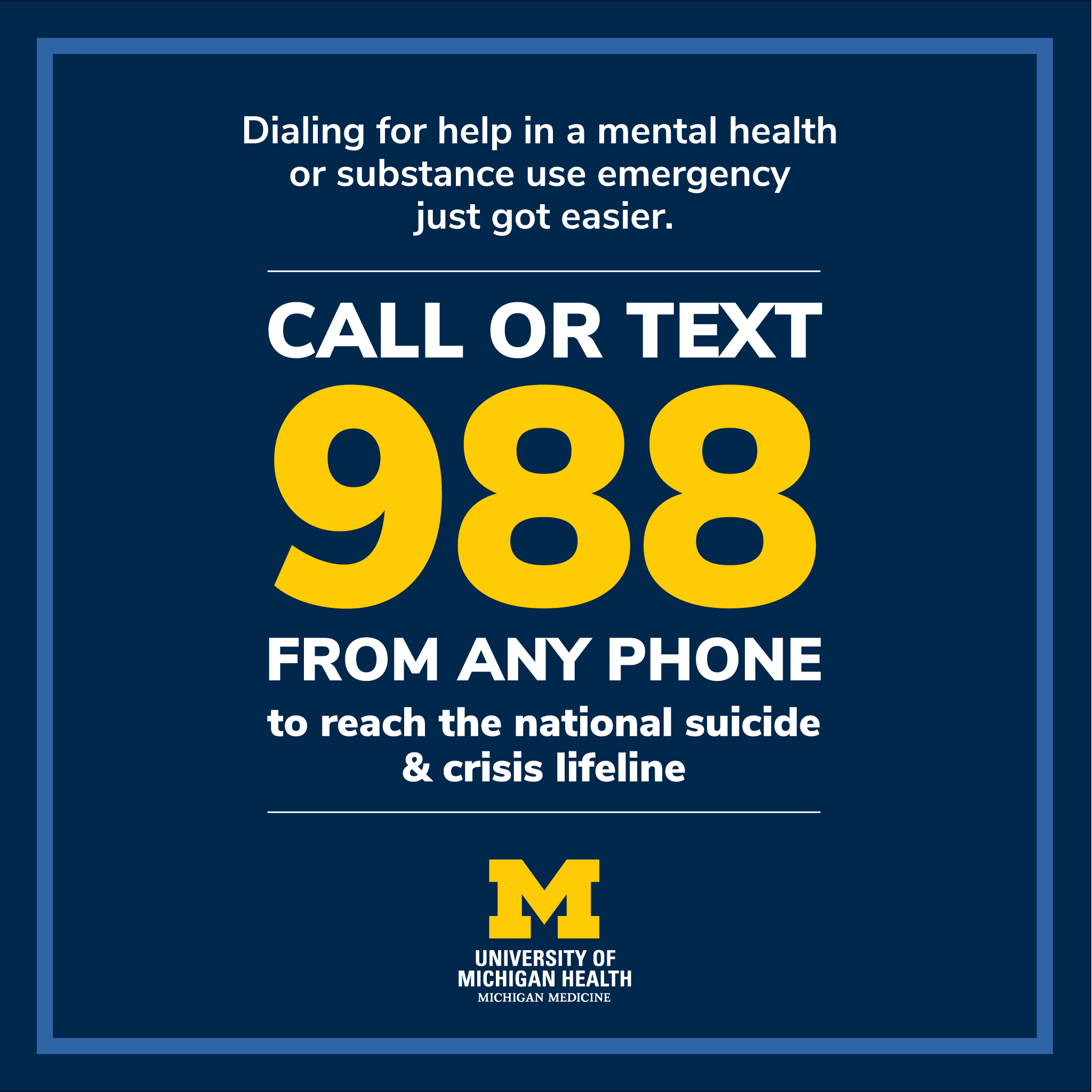
If you, your child or someone you know is having a mental health crisis or considering suicide, contact the national 988 Suicide and Crisis Lifeline by calling or texting 988, or visiting 988lifeline.org for crisis chat services or for more information.
If you are concerned that you or someone you know might have an eating disorder, the National Eating Disorders Association offers help by webchat, phone and text during certain hours.