MAPLE
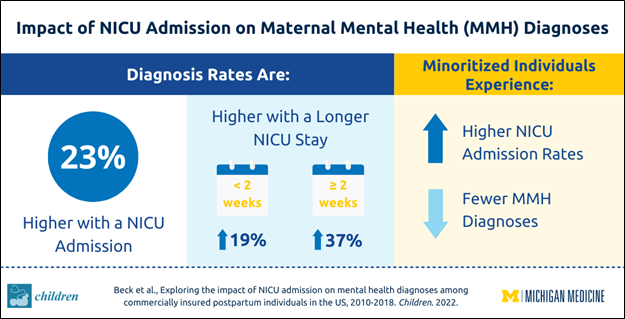
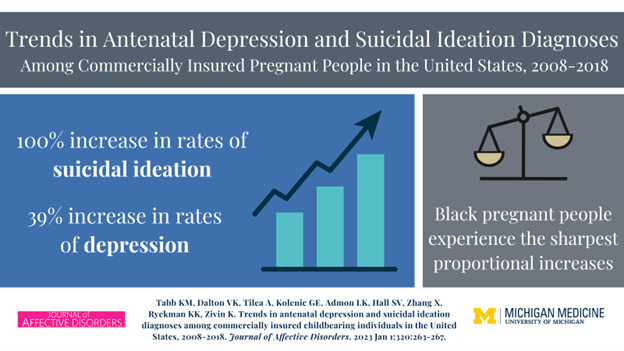
Through our work on the MAPLE project, we assess the impact of mental health policy changes on maternal mental health utilization, expenditures, and maternal mental health outcomes including suicidal ideation and self-harm, delivery outcomes, and overall health services utilization.
POPLAR
In POPLAR, we assess how behavioral health policy changes impact severe maternal morbidity.
BIRCH
In BIRCH we assess the impact of behavioral health policy changes on opioid prescriptions, diagnosed opioid use disorders, and prescription treatment for those disorders. We investigate how these policies impact chronic pain and suicidality, and delivery and infant outcomes like NICU admission and adverse birth outcomes. We also analyze how behavioral health policies impact maternal and infant health services utilization and expenditures.