In early March, the daily routines at Michigan Medicine changed dramatically.
As the health system prepared for a wave of COVID-19 patients, teams worked to rapidly expand ICU capacity and even develop new units to isolate infected patients. At the same time, certain activities not critical to caring for patients ramped down.
Among activities ramping down was most of the laboratory research at the University of Michigan: Experiments were frozen, labs went dark, and laboratory personnel isolated in their homes to avoid contact with COVID-19 and to preserve PPE.
Dr. Marilia Cascalho and Dr. Jeffrey Platt, a research team specializing in transplantation immunology and biology, continued working, however. They had pivoted to COVID 19-related research in early February and are now operating under a priority authorization with a grant from the Frankel Cardiovascular Center.
A new pandemic, a familiar viral profile
The trigger for the pivot wasn’t a case of COVID-19 at the hospital, or even in the state.
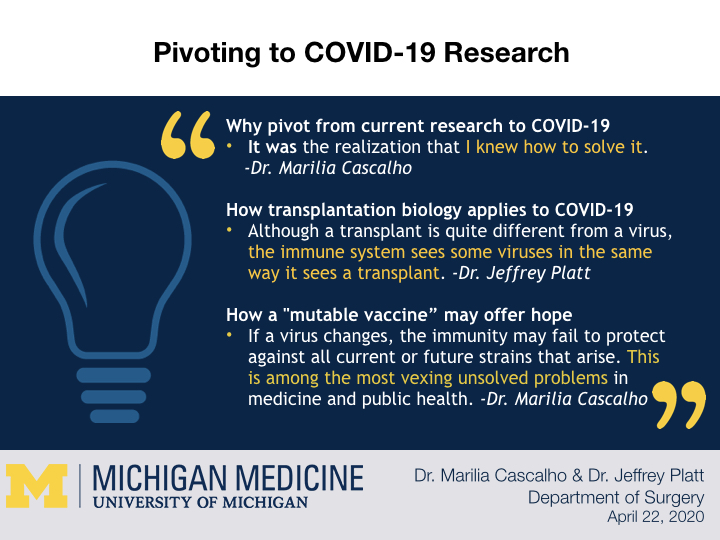
“For me it was the realization that I knew how to solve it,” Cascalho said.
If that seems like a bold statement, familiarity with Cascalho’s work might explain it.
Some years ago, Cascalho invented what she calls "the mutable vaccine”: A genetically-engineered vaccine that upon delivery into the body undergoes mutation in much the same way as some viruses. The vaccine thus anticipates some of the genetic changes viruses might undergo, potentially alerting the immune system to those changes.
When the problems associated with COVID-19 infection first became apparent, Cascalho felt like many others that the best solution would be an vaccine that would prevent infection.
However Cascalho knew that coronaviruses are among those that can rapidly mutate, giving rise to new strains. She feared even the most effective vaccine against a strain of COVID-19 existing today might fail to protect against new strains that emerge as the virus spreads widely in the population or passes between humans and animals.
Dr. Cascalho's fears appear justified as recent days have brought alarming reports about emergence of new strains of COVID-19.
“Conventional vaccination can be remarkably effective against genetically stable organisms yet frustratingly ineffective against organisms like HIV and hepatitis c that can mutate and diversify.
“When you vaccinate a person, you generate immunity to the virus that existed at the time the vaccine was made, but if that virus changes readily, the immunity may fail to protect against all current strains or future strains that arise. This is among the most vexing unsolved problems in medicine and public health,” Cascalho said.
Cascalho's first mutable vaccine was designed for HIV. She has shown that the vaccine could anticipate new HIV variants that actually developed in people and that it can generate protective immunity in mice. The vaccine does this by entering immune cells known as "B cells," which can produce the enzymes viruses use to generate mutations. Once inside B cells, the vaccine mutates as quickly as a virus generating new versions of viral genes that might develop during an infection. The vaccine is not a virus, so the new genes merely produce one or a few viral proteins without generating organisms.
The vaccine has an adaptation that Dr. Platt devised to provoke immunity against the new proteins. This added substance prods the immune system to target and ultimately destroy cells producing the new proteins. The vaccine remains because, like a mutable virus, it changes more rapidly than the immune system. If a virus were to enter the picture after the vaccine had been given, it would be confronted by an immune system poised to attack some and perhaps many of the variants it might generate.
“It means we created a vaccine that mutates with time, potentially anticipating and protecting against the changing forms of a mutable virus,” Cascalho said.
The mutable vaccine offers up a few potential modes of therapy.
Direct vaccination with the mutable vaccine as described above is one. The mutable vaccine can also be used in cell cultures to generate variants that potentially predict how a virus might change and provide a source of antigen (perhaps for conventional vaccination) before the changes actually arise in the virus. Finally, the mutable vaccine could be used in animals to generate antibodies that could be given like a drug when new versions of the virus emerge.
Transplantation biology research in a new context
Transplantation biology being their core research area, Cascalho and Platt investigate immune and inflammatory processes that harm organ transplants. Some of the processes could offer clues about how to attack the COVID-19 virus or how to control the inflammatory injury thought to underlie the most severe cases of COVID-19.
Drs. Platt and Cascalho were already investigating the immune boosting substance in the mutable vaccine as a potential contributor to rejection of organ and tissue transplants. As part of that effort, they developed a boosting drug and an inhibitor for their early transplant studies. It was a small step to ask whether an immune booster could help eradicate a virus or whether the inhibitor stem the inflammation proved by the virus.
The team has another way to stem the impact of inflammation troubling some patients with COVID-19.
“Years ago we discovered that organs or tissues can acquire resistance to immune or inflammatory injury and recently figured out how transplants do so. Although a transplant is quite different from a virus, the immune system sees some viruses in the same way it sees a transplant and vice versa.
“A great challenge for the immune system is how to destroy a virus without destroying the organ or tissue that harbors that virus. In most cases, the immune system collaborates effectively with the infected organ or tissue to rid an infection while allowing the organ or tissue to recover. In some COVID-19 infections, as in some transplants, this collaboration fails.
"If we find that severely afflicted lungs, like transplants, lose the capacity to resist immune and inflammatory injury, we have a set of agents we devised to help with that problem,” Platt said.
As a respiratory virus, COVID-19 sets its sights on the lungs. In severe cases, the inflammatory response runs amok, impacting the heart and other organs and resulting in serious complications or death.
Before the COVID-19 pandemic, Cascalho and Platt were testing a recombinant protein that they found boosts immune responses to viruses. They had been testing that protein as a way of helping to boost immunity to cancer. To apply their discovery in transplantation, they developed an inhibitor of the protein, hoping to suppress the powerful responses transplants evoke. The COVID-19 pandemic persuaded them to return to the original aim of using the protein to raise immunity to viruses.
“If you view the virus as being like a foreign organ, some of the rules that we’ve learned over the years potentially apply just as much to this virus. The technologies we propose are a direct extension of the work we were doing in transplantation,” Platt said.
There is strong but still limited evidence that administering antibodies taken from patients who recovered from COVID-19 may be helpful in treating severely afflicted patients, Platt said. However, administering antibodies can have a downside. Some of these antibodies could promote excess inflammation and a harmful response. Administered antibodies also might block the immune system from developing immunity against the part of the virus the antibodies bind.
To give antibody therapy the best chance of helping rather than harming patients, Dr. Cascalho is experimenting with separating the antibody-producing cells to potentially retain helpful antibodies and remove harmful antibodies. Cascalho is collaborating with Dr. Millie Samaniego, a nephrologist at Henry Ford Health System, to acquire blood from recovered COVID-19 patients.
Research during the new normal
While the pivot to COVID-19 research has been easy in some ways, the research comes with challenges unique to working in an environment altered by a pandemic.
The pace of work is slower due to restrictions put in place for the safety of employees and patients, for example.
For example, only two people instead of a typical team of five can be in the lab at a time to maintain physical distancing. Therefore, Cascalho and Platt diligently schedule members of their team to make sure no more than two show up at a time.
One thing that hasn’t changed is the need for flexibility based on how experiments track and when supplies are available.
“I hope to be getting blood from patients soon. Whenever the blood is available we’re going to work. Day or night, anytime,” Cascalho said.
##
By Colleen Stone