The University of Michigan hockey team will hold its fourth annual ALS Awareness Game (#IceALS) this Friday (Dec. 6) when it competes against Penn State University at Yost Ice Arena. The battle on the ice between the Wolverines and Nittany Lions will be televised nationally on Fox Sports 1 at 8:30 p.m. The event also presents an opportunity for two old friends in the ALS scientific community to come together.
A U-M neurologist since 1988, Eva Feldman, M.D., Ph.D., mentored Zach Simmons, M.D., from 1990-92 before he moved onto a successful career at Penn State Health. They have maintained their friendship for nearly 30 years and they each lead their respective university’s multidisciplinary ALS clinics.
Drs. Feldman and Simmons caught up with each other earlier this week to talk about the genesis of Ice ALS, their history together, and the present and future of ALS research and treatment.
The Inspiration Behind #IceALS

Dr. Feldman: A few years ago, I diagnosed a young man with ALS named Scott Matzka, who had been on U-M’s national championship hockey team in 1998. The hockey coach at the time, Red Berenson, was very devoted to Scott and to all of his players, so when he learned that Scott had developed ALS, he and his hockey staff and alumni wanted to do something special for him. Four years ago they began dedicating a hockey game each season to raise awareness for ALS and called it Ice ALS. Scott was alive when we did the game last year, but this will sadly be the one-year anniversary of his death. Scott always had an enormous amount of courage and optimism. He was selfless and very much wanted to see ALS research move forward. He was an outstanding young man and I had the pleasure of getting to know him, his wife and two children.
When we knew Penn State was coming into town this year, we thought this event could be a great opportunity to showcase the great work that both Michigan and Penn State have accomplished in the fight against ALS. We’re so excited that you are coming to visit us.
Dr. Simmons: Eva as you were talking, it struck me that to make ALS research truly successful it needs to be approached from several different angles. There’s the most basic science research that helps us understand the underlying mechanisms of the disease. There’s the translational research that puts those research discoveries into opportunities to develop new therapies. There is also the actual management of our patients and conducting clinical trials. In addition, patients and caregivers come with different resources. As physicians and ALS center directors, we are looking for more effective treatments and to help these patients and their families manage this devastating disease.
The Beginnings of a Long Friendship, It Starts with a Fellowship
Dr. Feldman: We met when you became my fellow in 1990. Usually our applicants for fellowships come directly from doing their residency, but you had actually practiced neurology for four years. Your two-year fellowship included doing research in your second year. I actually remember your fellowship. I was a very young attending. I finished my own fellowship in 1988, so I was only two years out. You had more experience than me as a neurologist. I was your attending, and you my fellow, though what I really remember was that it was more of an equal partnership.
Dr. Simmons: I really think the big difference was, Eva, that you had a research background, whereas I did not. My hope in taking that fellowship position was that I would be able to get a better understanding of the research process, and perhaps become involved in research at the clinical level, because that is something I hadn’t been exposed to.
Dr. Feldman: That worked out well! When did you develop your interest in ALS? When you were a fellow? Or, was that when you moved on to Penn State?
Dr. Simmons: It was really when I moved to Penn State. At Michigan, you and Dr. Jim Albers gave me a lot of opportunities to look at Michigan’s long track record of taking care of people with CIDP (Chronic Inflammatory Demyelinating Neuropathy). The clinical research I did at Michigan involved a lot of review of those CIDP records, but at that time Michigan didn’t have an active ALS program. When I came to Penn State Health, the department was very small and they didn’t have any other neuromuscular specialist, so they started sending all of the ALS patients to me. The training at Michigan was great. At Michigan, I was able to perform the initial diagnosis of ALS, and learn how to interpret the EMGs (electromyography). That’s what really made me comfortable when I came to Penn State Health and established this program here.
Since my fellowship, you and I have kept our ALS ties close. We have had you give grand rounds at Penn State Health, for example, and we worked together on the stem cell study where I was on the safety monitoring board and you were the principle investigator.
The Direction of Current ALS Research
Dr. Feldman: Today, I would say the ALS Center of Excellence at Michigan Medicine is focused on three areas. The first is understanding the role of the environment on disease onset and progression. We really feel that there is likely an environmental component that tips one over to developing this disease. Michigan has the highest prevalence of ALS of any state in the country. We are both an agricultural and an industrial state, and are a highly polluted state. Michigan still has over 65 uncleaned Superfund contaminated sites. We have found that ALS patients have higher levels of pesticides in their blood as compared to healthy individuals. Our work shows an association, but we have yet to show a causation. We are extremely interested in that.
Secondly, I am happy to say that we were just awarded a brand new 5-year RO1 grant to expand our work on environmental risk with ALS. An additional component will investigate if there is a polygenic risk to develop ALS. If there are two people equally exposed to the same environmental pollutants, is one more likely to develop ALS or another neurodegenerative disease? We are developing polygenic risk scores, particularly by looking at enzymes that are involved in detoxification of organic pollutants.
Our third area of interest is the investigation of the role of the immune system in ALS. Our work has shown a clear connection to immunity and the disease. We have looked at the white blood cell profile of nearly 600 patients and found you can correlate their immune status with the state of the disease. We can also correlate certain sub-types of immune cells, called natural killer cells. If you have high levels of natural killer cells you automatically have a very progressive disorder. We are interested in repurposing a drug that specifically focuses on natural killer cells. This drug is called Tofacitinib, which attacks these cells and already has FDA approval for use in other diseases.
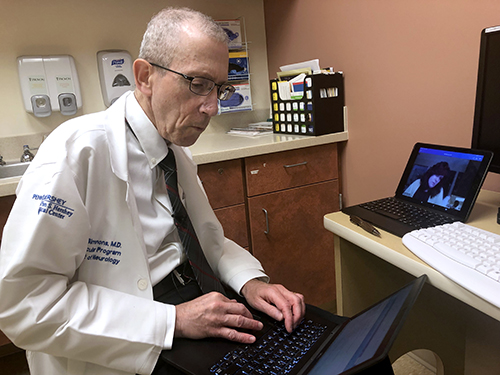
Dr. Zachary Simmons using telehealth
Dr. Simmons: In many respects there are a lot of parallels between the populations of Michigan and Pennsylvania. Both are fairly large states with major metropolitan areas. They also have large agricultural and industrial areas. We have not looked at those factors here at Penn State Health. Should you at some point have data that warrants a broader look at patients in another geographical area, we are of course happy to contribute to the work that you are doing.
At Penn State Health, we have focused on telehealth based on an article we published a few years ago, that surveyed patients with ALS who went to multidisciplinary clinics. The patients say the strengths of those clinics are those you might imagine: the multidisciplinary care, the high level of expertise, the availability of research. The drawbacks were that it usually involves long travel time and exhausting days—a typical ALS clinic visit lasts anywhere from 2-4 hours. Telehealth has emerged as a way to preserve the benefits of a multidisciplinary clinic, while lessening the burdens on patients. We have implemented this in three ways.
First, we use telehealth as a substitute for the multidisciplinary visit, so patients stay in their homes and connect with us when we have an ALS clinic day. In our ALS clinic, we then have the patient on the computer screen and the multidisciplinary team members come in one at a time to do their interaction virtually. Secondly, we have also used it for one-on-one care visits with our health care team members. If a patient has a particular concern, sometimes a face-to-face visit will work better than a telephone call. Then thirdly, we have tried to reduce the length of the multidisciplinary visit. For example, if we can accomplish the nursing or the social work portion of the visit beforehand remotely, then the actual visit to the clinic could be shorter. The patients and their caregivers have told us that the biggest positive of telehealth is that it is a much less stressful day for them. They are in their homes, they are in their comfortable clothes, their spouse hasn’t had to drive on the interstate for hours and they aren’t as tired. The patients seem different on the days they have a telehealth visit because they seem so much more relaxed and able to interact with us. We see this as one of the greatest benefits.
Dr. Feldman: I’m very excited to hear what you have done on telehealth because we have just started to get into that area. There are going to be a lot of people in the telehealth space at Michigan who have decided to come hear you speak this Friday. We have not embarked on telehealth the way you have and we really feel that it is the wave of the future.
We have such a nice intersection of ALS clinics, I think. While I’m in the laboratory trying to discover a new drug, you are in the clinic helping to determine the best way to take care of those patients. What are the stressors and what are the non-stressors for the patient and the caregiver? When to start a feeding tube? When to intercede for early ventilatory care? We come to the same disease from two different angles, but with very much the same goal. Our goal is to improve the quality of life of these patients. You know we are trying to find something that slows disease progression and you have shown in your research that a high-quality, multi-disciplinary center can actually improve and enhance the patient’s quality of life, and lengthen their life span.
A Vision for the Next 5 Years
Dr. Feldman: The design for clinical trials is changing. The new design allows for more patients in a clinical trial. In the next 3-5 years, I would like to see a faster track of research from the basic science lab to the clinic, using these more innovative trial designs. I think we need to be a little more facile with our clinical trials, a little lighter on our feet, to get them off the ground, and to move them forward.
Dr. Simmons: I agree 100% with what you said. The only thing I would add would be that only a small percentage of individuals with ALS currently participate in clinical trials. One hope to increase that number would be to reduce the burden on the patient by the use of technology. For example, rather than having visits to an ALS center at a particular frequency for participation in their trial, some of those visits could be done at home–measuring things such as grip strength, changes in voice or pulmonary function testing, or certain aspects of gait and falling. There are a number of ways of trying remote monitoring to reduce the burden on patients and increase enrollment of clinical trials.
And of Course a Little Rivalry
Dr. Feldman: We are so excited about the hockey game. We will play each other, not fight each other. At least, Dr. Simmons, I have a hockey jersey. You don’t have a hockey jersey.
Dr. Simmons: Let’s say that goes into the category of I’m working on it. I will see what I can do. As an undergraduate (at Dartmouth) I actually went to most of the home hockey games, but it’s been a few years. This will be the first time I will get to see Penn State play hockey, since their varsity team is relatively new. I can’t wait!
