Earlier this year, Michigan Medicine and the NeuroNetwork for Emerging Therapies welcomed Assistant Professor of Neurology Brett McCray, M.D., Ph.D., from Johns Hopkins University.
"Michigan Medicine is incredibly fortunate to have Brett join us from Johns Hopkins," said Eva Feldman, M.D., Ph.D. " Not only will greatly impact patients' lives in the clinic, but I truly believe that his research will change the game in our treatment of neuropathy. He offers great hope for the future of the field."
We sat down with Dr. McCray to learn more about the man behind the white coat, and his research.
Welcome to the NeuroNetwork. Could you please explain a little about your work here at Michigan Medicine?
Two days a week, I see neurology patients and help direct the Charcot-Marie-Tooth disease (CMT) clinic. CMT includes a large group of different forms of inherited peripheral neuropathy, and it is actually the most common genetic neurological condition worldwide.
The rest of my time is spent on my research, which is focused on investigating forms of hereditary neuropathy (as opposed to acquired neuropathy like diabetic peripheral neuropathy). I believe that if we better understand how specific genetic mutations cause neuropathy, we will not only be able to identify treatments for affected CMT patients, but our research may also provide insights into pathways that are important to nerve health in general. Such insights into fundamental aspects of nerve biology and health can then be applied across neurologic research.
Tell us more about your lab and research.
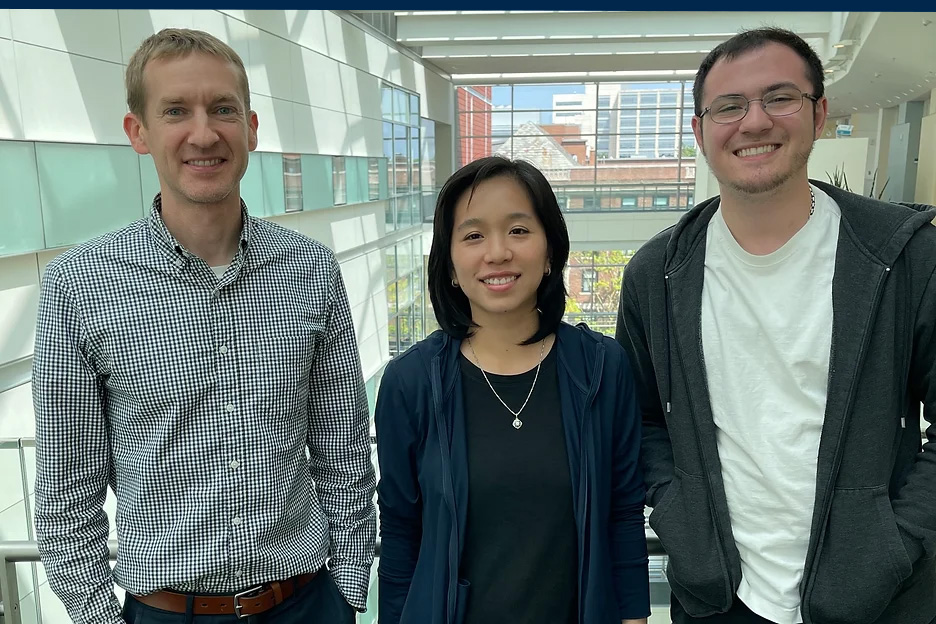
Right now, in my lab, I have a fellow and a research technician working with me, but we plan to grow very soon. Linh Vo, Ph.D., is a postdoctoral fellow originally from Vietnam who just completed her Ph.D. training at Wayne State University where she worked on a form of inherited muscle disease. Our technician, Gage Kosmanopolus, was born and raised in Michigan. Grand Blanc to be exact. He recently graduated from Michigan State with a degree in biochemistry and molecular biology.
As for research, there are over 100 genes connected with hereditary neuropathy, but we focus on TRPV4, which is the gene that causes CMT type 2C. It is unique because it is the only ion channel that is mutated in CMT, which makes this form of CMT potentially treatable with drugs that alter the channel’s activity. So, by studying how TRPV4 causes nerve degeneration and the pathways it activates, I believe that we can develop a successful treatment for CMT2C and also identify ways in which TRPV4 drugs could be useful for other neurological diseases.
Does the type of neuropathy you study present differently in patients?
Most neuropathy is what we call “length dependent.” In other words, it often starts in the toes and feet of patients and progresses up the body. So, most research on CMT has focused on measuring this pattern of disease onset and progression. However, the patients with CMT2C that I study usually don’t follow this rule.
They often have thigh weakness and shoulder weakness, and a high percentage of them have vocal cord weakness as well. This affects voice and breathing, which can make a common cold pretty dangerous.
How did you become interested in hereditary neuropathy and this specific type?
I think it's interesting that this is where I ended up because I did a research project as a graduate student on a different form of CMT and wasn't particularly interested in the disease itself -- it was the normal biology of a particular gene connected with it that I found intriguing. I’ve always been interested in pathways of neurodegeneration, and it made sense to me that starting with genetics was a good way to get a sense of where the basis of the problem lies.
So, as a grad student, I studied this CMT gene, but when I went off to residency, I forgot all about the disease. Then, as a neuromuscular fellow many years later, I began to work with Charlotte Sumner, MD, at Johns Hopkins, who studies and sees patients with CMT. Through her mentorship, I suddenly was enthralled by the CMT patient population. I also realized that since there are currently no viable treatments available for any form of CMT, there was a strong need for more research in this field.
What brought you to Michigan Medicine?
I was at a point in my career where I was trying to grow my lab program, and I found Michigan Medicine to have a very supportive environment for what I was trying to accomplish. I was looking for a place that values physicians and scientists equally, and here it is ingrained in the culture. They recognize that being a physician-scientist is a worthy enterprise. Clearly, there are a lot of people here who have been successful in this career path. So, I decided that Michigan Medicine provided the foundation and environment that would take me to that next step.
So how do you feel about Ann Arbor?
It’s very safe and family-friendly, so it has been easy to live here so far. I live close to work, so I can bike in, which I really enjoy. Surprisingly, there is a lot about life in Ann Arbor that has parallels to life in Baltimore, where I lived when I was at Johns Hopkins. But the Ann Arbor version is always easier and usually more enjoyable. For instance, my family always enjoyed eating at Shake Shack in Baltimore, but it was impossible to park nearby, and finding a seat was always a challenge. Here, it takes about 30 seconds to park, there is a ton of seating, and there's a foosball table! That type of thing keeps happening, where Ann Arbor makes things less stressful and more family-friendly. I have three kids, which was a bit of an oddity for faculty members at Johns Hopkins, but here it seems very common.
You said there was a story related to your work that your kids love to hear.
I always thought my eventual career would involve something artistic. When I was starting college, my top career choice was architecture. But when I started interviewing for architecture programs, I was cautioned that being an architect required a lot of education...8 years after high school! That seemed unthinkable and I decided architecture wasn't for me. But look where I ended up -- MD, PhD, internship, residency, fellowship, about 17 years of training after high school. I guess it doesn't matter how long it takes when it's something you love. I still enjoy art in my spare time, and it's something I can share with my kids. I painted two murals in our house in Baltimore and I hope to eventually do the same here.