From the Michigan Medicine Health Lab blog:
How a high-fat diet may alter the gut microbiome and lead to peripheral nerve damage
A study in mice establishes a connection between diet, microbiome and nerve health
Author|Patricia DeLacey
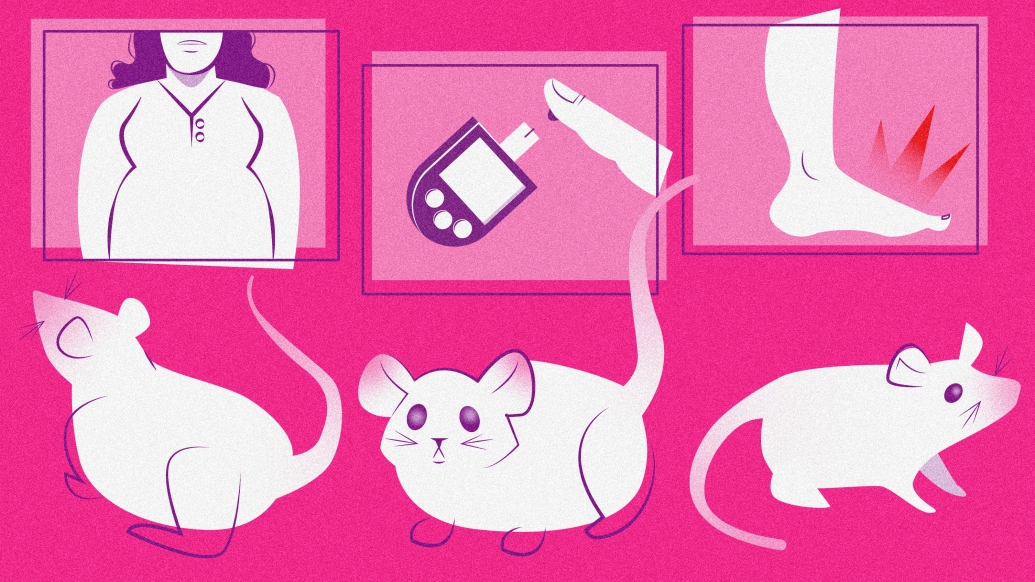
Obesity, prediabetes and type 2 diabetes are global epidemics affecting hundreds of millions of people worldwide.
In large part they’re driven by the overconsumption of the “Western diet”, which is known for being rich in saturated fat (e.g., pre-packaged foods, red meat, refined grains, fried foods.)
Sadly, these metabolic disorders have cascading detrimental effects across the body.
One common complication associated with these conditions is peripheral neuropathy, a disorder of the peripheral nerves that affects the hands and feet which can cause chronic pain, weakness, tingling, numbness, balance issues and can even lead to amputation.
Although the association between metabolic disorders and peripheral neuropathy is well known, there are no studies showing how they are linked, explains Mohamed Noureldein, Ph.D., a postdoctoral fellow at the NeuroNetwork for Emerging Therapies in Michigan Medicine’s Department of Neurology.
But Michigan Medicine-led research suggests that the gut microbiome, the trillions of bacteria that live in your gut, may serve as the link between a high-fat diet and metabolic and nerve health.
The results are published in Microbiome.
The findings
Using genetic sequencing technology, the researchers found the microbiome was different between mice fed a high-fat diet and those fed a standard diet.
In the high-fat diet mice, there were several microbial groups associated with metabolic health and peripheral neuropathy.
These mice also displayed a “slowdown of the nerve condition velocity, which tells us how fast the electrical impulses are transferred along the nerve,” which indicated injury to both motor and sensory nerves.
“The impact of a high-fat diet on gut microbiome structure is well established, but these results provide some of the first evidence that peripheral nerve health correlates with distinct microbiome signatures,” said Eva Feldman, M.D., Ph.D., James W. Albers Distinguished University Professor and Russel N. DeJong Professor of Neurology.
Several peripheral neuropathy-associated microbes from the high-fat diet group were linked to changes in sciatic nerve gene expression related to inflammation, lipid metabolism and antioxidant defense.
The microbial connection to the sciatic nerve is important as damage to the sciatic nerve indicates a severe peripheral neuropathy case.
“When the sciatic nerve is affected in metabolic syndrome and obesity, it is the worst-case scenario,” Noureldein said.
“In peripheral neuropathy the small sensory nerves are affected first before large motor/sensory nerves like the sciatic nerve. The sciatic nerve is affected at the last stage which is why we chose to study it.”
This newly discovered mechanism correlating differences in microbiota to peripheral neuropathy has translational implications for the future treatment of peripheral neuropathy in humans.
When treating peripheral neuropathy, “we don’t only need to change the diet, we also need to change the microbiota,” said Noureldein.
Potential treatments could include probiotics or fecal microbial transplants prescribed along with diet changes to promote a healthy community of gut microbes.
Other potential treatments involve intervening before the microbiome affects nerve health. Drugs could be developed to inhibit metabolites from peripheral neuropathy-associated microbes in the blood before they reach the nerve.
Another avenue could be to employ anti-inflammatory drugs or drugs that act on identified metabolic pathways to treat or delay the development of peripheral neuropathy induced by metabolic disorders.
Next steps
The work on this exciting topic is ongoing.
Future studies in mice will further probe the mechanism by directly assessing the effect of microbiota on nerve health without diet changes and test therapeutic opportunities by evaluating whether supplying probiotics to mice fed a high-fat diet will reverse the effects of peripheral neuropathy.
“This new insight into a gut-microbiome-peripheral nervous system signature in peripheral neuropathy lays the groundwork for future therapeutic opportunities for this painful disease in obese, prediabetic and diabetic individuals,” said Feldman.
In addition to Noureldein, the research team included co-lead authors Kai Guo, Ph.D., and Claudia Figueroa-Romero, Ph.D., senior author Eva Feldman, M.D., Ph.D., Lucy Hinder, Ph.D., Stacey Sakowski, Ph.D., Amy Rumora, Ph.D. of the Columbia University Department of Neurology, Hayley Petit, Masha Savelieff, Ph.D. and Junguk Hur, Ph.D. of the University of North Dakota Department of Biomedical Sciences. All but Hinder, Rumora and Hur are part of the Michigan Medicine Department of Neurology.
Paper cited: “Gut microbiota in a mouse model of obesity and peripheral neuropathy associated with plasma and nerve lipidomics and nerve transcriptomics,” Microbiome. DOI: 10.1186/s40168-022-01436-3