If you had a procedure in your toolkit proven to help people get to a healthier weight and mitigate or even resolve their diabetes, high blood pressure and high cholesterol, would you use it?
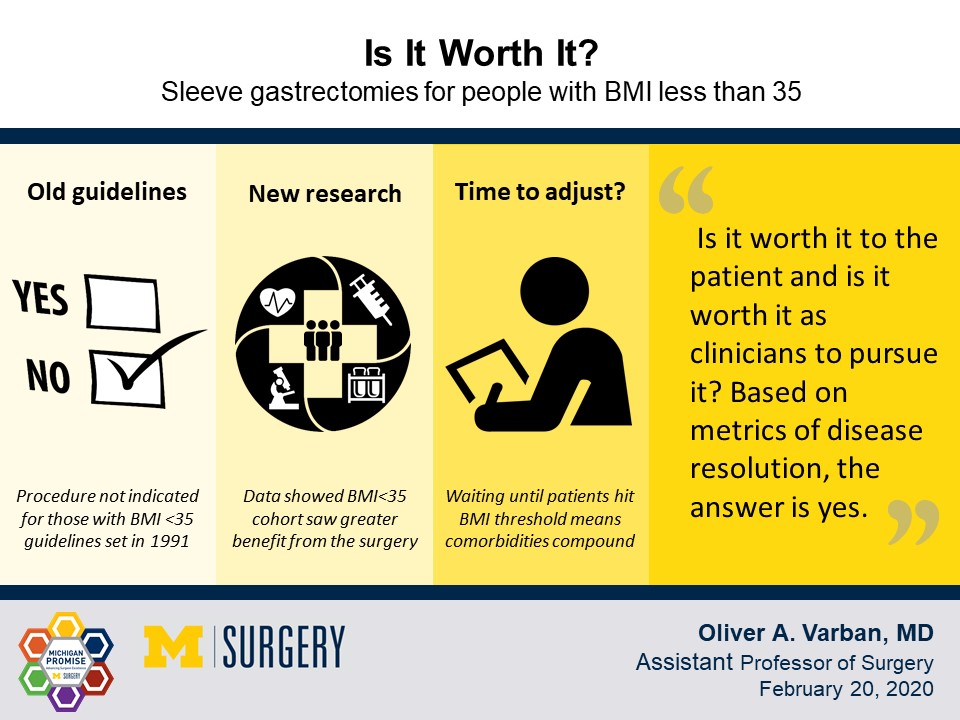
If those people had a body mass index lower than 35 kg/m2, you might not have a choice; guidelines established by the NIH in 1991 don’t indicate sleeve gastrectomies in people with a BMI lower than 35, even if they have associated medical conditions. Therefore, most health insurers won't cover the procedures in that population.
The big why
Dr. Oliver Varban, associate professor of surgery at Michigan Medicine, has seen the benefits of sleeve gastrectomies, which involve removing a part of the stomach laparoscopically. The procedure restricts caloric intake and kicks profound metabolic changes into effect.
“One thing that blows everybody's mind is that people come off of their diabetic medication, completely eliminating their need for insulin within weeks or months before they even maximize their weight loss,” Varban said.
While the mechanisms for those metabolic changes aren’t completely understood, the upsides are clear: The classic obesity-related diseases—diabetes, high blood pressure and high cholesterol—go away or are less severe.
“How curious, we have an intervention that treats all of this but its focus and its use is very narrow and we don’t know what the impact of it is on a more diverse population because we don't have the opportunity to study that because we can’t meet the indications for that,” Varban said.
Varban and colleagues found a way, parsing data from the Michigan Bariatric Surgery Collaborative. They identified 1,073 patients who underwent sleeve gastrectomies at hospitals within the collaborative while their BMI was less than 35. That slice represented 2.4 percent of all sleeve gastrectomies performed at the affiliated hospitals from 2006-2018.
Those patients were able to have the surgeries either because they paid out of pocket or because they were above the BMI threshold before surgery. (Demonstrated weight loss is typically required before bariatric surgeries, to improve surgical outcomes and get patients to adopt habits that will serve them well after the surgery.)
They fared as well or better than those undergoing the procedure at a higher BMI. In other words, there’s no magic to the number 35 in the context of this surgery and that there’s no good clinical reason the guideline should stand. That finding was published in the Surgery for Obesity and Related Diseases.
Outcomes don’t lie, but BMI sometimes does
Varban was struck by what he saw in the data. Patients undergoing the surgery at the lower BMI were older and actually had more comorbid conditions than the patients undergoing the surgery above the BMI threshold.
“It wasn’t just young people trying to lose weight to fit into their wedding dress,” Varban said.
While the cohort looked older and sicker before surgery, with higher rates of diabetes, high blood pressure and high cholesterol, they benefited similarly in terms of comorbidity results. They discontinued medications for their metabolic conditions at similar rates.
In other ways, they overachieved. They were more likely to achieve a healthy BMI and had markedly higher body image scores and higher overall satisfaction with the procedure.
The outcomes among this lower-BMI group point to the pitfalls of BMI as the primary measure for metabolic health, Varban said.
“If I see this operation as something that treats metabolic disease, then we need a better calculator to measure metabolic risk and metabolic severity. BMI is one, but it should be weighted in a different way.”
Why wait to see the benefits?
Sleeve gastrectomies are one of the most common bariatric procedures, with the fewest complications and some of the most profound metabolic benefits that affect downstream health.
“Why focus on these comorbidities? Because these are the things that give people strokes, heart attacks and need transplants,” Varban said.
He pointed to the eye-popping figures regarding patients coming off of diabetes medications following the procedure as another reason not to wait; nearly 80 percent of patients discontinue oral medications and more than 60 percent discontinue insulin use.
“There’s no other intervention that offers that and I’m sure that patients would love to not give themselves insulin. The other thing is how often people get to a normal BMI. Why do we need to wait and ignore it and wait to a point where it won’t even help?”
Defining worth
Varban’s paper asked whether sleeve gastrectomies are worth it for people with a BMI less than 35.
“Worth it is a loaded term because it has to do with what you consider value and what you consider cost. Is it worth it to the patient and is it worth it as clinicians to pursue it? Based on metrics of disease resolution, the answer is yes,” Varban said.
Economically, it’s more complicated. It’s hard for insurance companies to square the long-term benefit with the large up-front cost. The procedures range from $10,000-$20,000 depending on the hospital, Varban said.
“What is the ROI on that? It’s coming off of medications. Here’s the problem with that. The medications are cheap and it’s easy to prescribe them, easier than surgery,” Varban said.
He points to other benefits that are harder to quantify in a short-term focused system: A person with a high BMI is likely to have a higher risk of complications from any surgery they have. Conversely, any surgery someone has after bariatric surgery is likely to bring fewer complications with it.
An opportunity to further diversify study cohorts
The paper highlights how important diversity is in medicine, at the clinical level and the research level, Varban said. Some of the earlier research that informed the current guidelines for sleeve gastrectomies skewed heavily toward white women with BMIs over 45, for example.
“We don’t only treat those types of patient populations...other research that shows the incidence of metabolic disease, can actually happen at much lower BMI in certain populations, particularly in Asian populations,” Varban said.
When the research pool is more diversified, updated guidelines could open the procedures up to more people, according to Varban.
Related link: The Michigan Bariatric Surgery Collaborative has developed a Bariatric Surgery Outcomes Calculator that can predict a patient's individual weight loss, comorbidity resolution and complication rate after bariatric surgery. Doctors can use it to start the conversation about what bariatric surgery is and does.
##
By Colleen Stone