This past year, family medicine residents had the opportunity to design and conduct original clinical research, with guidance and support from faculty mentors and staff. The resident research program, led by assistant professor Katherine J. Gold, M.D., M.S.W., M.S., paired residents with research faculty in the department. Over the course of the 2016-2017 year, residents developed a research question, designed and conducted their study, and presented their work at regional, national, and international conferences and prepared their work for peer-reviewed publication. The program provided exposure to the academic and clinical research process, from start to finish.
First steps in clinical research
Third-year resident Yujing Lin, M.D., reflected on her first experience with clinical research, "My prior background in research was bench work, molecular research, where you are doing some cloning and isolating DNA. This was the first time I'd done more, clinical research, where you have a clinical question that you’re trying to answer."
"It's very different in that, there’s not always a set protocol on how to do it. And you have to go through the IRB. Especially if you’re interacting with patients and providers, and you have to think about ways to ensure confidentiality. There’s just a lot of other aspects [of clinical research] that I didn’t think about until I was working on the project."
Dr. Lin's research emerged from a real concern for her chronic pain patients. "In medical school, we learn that cognitive-behavioral therapy (CBT) is really helpful for treating chronic pain, but I wasn't seeing it be prescribed very frequently, in real practice. So, I wanted to focus my project to study the prevalence of CBT referrals for chronic pain syndrome (CPS)."

Her interest in chronic pain management led to making a connection with faculty mentors, Suzanna Zick, N.D., M.P.H., whose research focuses on alternative therapies in the breast cancer continuum, and Jill Schneiderhan M.D., who recently published analysis in the Journal of the American Medical Association (JAMA) on chronic pain management in primary care. Zick and Schneiderhan helped Lin navigate the research world: From designing her survey and navigating IRB approval, to developing recruitment efforts that reached her target population.
Was Lin's observation of infrequent CBT referrals anecdotal, or could it be supported by data? Because cognitive behavioral therapy can come in many forms, ranging from psychotherapy sessions with a clinical psychologist to utilizing specific self-help books and web-based tools, CBT referrals are not clearly documented, and thus extractable, from most electronic health record (EHR) systems. Getting data on referrals would require going to the source: Primary care physicians.
Lin surveyed 86 primary care physicians in Michigan, distributing a web-based survey with questions that sought to establish self-reported CBT referral rates, as well as to describe physician demographic factors that might correlate with CBT referral rates, such as physician's gender, years of practice, and background knowledge of CBT.
"Overall, referral rates are pretty low," Lin found. "Only about a third of the survey responders said that they had ever prescribed CBT for fibromyalgia, migraine or low back pain. And out of that third, the vast majority of them--75% said they would refer CBT less than 40% of the time." The survey assessed respondents' background knowledge of CBT--like identifying the purpose and recommended frequency of CBT treatments, as well asking physicians to recall which diseases have shown evidence-based benefits from CBT treatment. Lin found that "there was a statistically significant correlation, in that respondents with higher knowledge scores tend to refer more often." Other demographic factors, like a physician's age, gender, and years in practice did not produce statistically significant correlations with rates of CBT referral. But Lin suspects there may be more demographic factors to uncover.
Before Dr. Lin dives deeper into the investigation, like with a nationwide survey of CBT referral in primary care, she hopes her resident research could have an impact on practice, at the local-level. "I think the first step is to try to promote these results in our own institutions, to find ways to make changes, and to then see if those changes have any measurable difference in our patient satisfaction." Paired with the recent JAMA piece, Lin and Schneiderhan make a strong case for pragmatic, patient-centered primary care research to address chronic pain and related issues, like the opioid crisis.
The end of the beginning
Third-year resident Deborah Phipps, M.D. brought her research to Washington D.C., presenting at the World Health Congress this past spring with her faculty mentor Justine Wu, M.D., M.P.H. You can find her research abstract published in the Journal of Women's Health. Dr. Phipps' research uncovered parental attitudes towards the availability of over-the-counter contraceptive pills. This spring, shortly after presenting her research at U-M Family Medicine Grand Rounds, Phipps' work gained attention from the Oral Contraceptives (OCs) Over-the-Counter (OTC) Working Group. The national coalition requested to hear more about Phipps' research as it filled a critical research gap in the implementation of over the counter access to oral contraceptives. Wu noted that the group was "impressed with how much Debbie has accomplished during her residency" and were eager to hear her final results.
The resident research project is just the beginning for Dr. Phipps. She plans to continue her research next year, as part of her Women's Health fellowship.
Leadership through sharing at STFM and the Michigan Family Medicine Research Day
U-M family medicine residents have shared their research projects at regional, national, and international professional conferences, including the Society for Teachers of Family Medicine (STFM) annual conference this past May and the Michigan Family Medicine Research Day. The department hosted a virtual STFM poster session, showcasing work from residents Leigh Morrison, M.D. and Anna McEvoy, M.D., as well as U-M medical student Manisha Rai. This post documents the line-up of excellent presentations and posters from U-M residents and faculty.
A number of residents presented their research at the Michigan Family Medicine Research Day, which was held on May 25 at Cleary University. U-M was strongly represented at the regional event, which brings together academic and clinical family medicine programs from across the state. Two of the resident projects won awards for Best Oral Presentation by a Resident, including Matthew Kittle, D.O. and Marian Deames, M.D. who won for their presentation “Family Physicians’ Knowledge and Beliefs Regarding the Health Effects of Added Sugar" and Anna McEvoy, M.D. for her presentation “Family Physicians and Provision of Immediate Postpartum Contraception.”

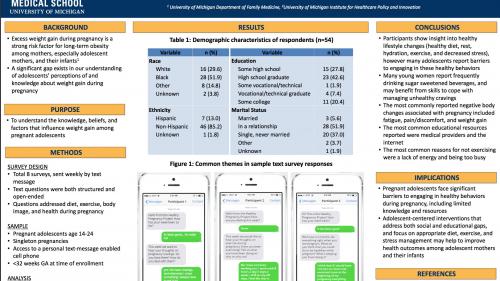
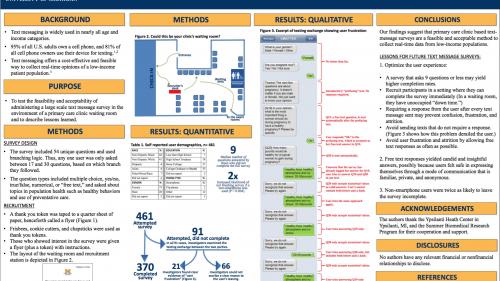
All four of these award-winning, nationally-recognized resident and student research projects were fueled by the seemingly inextinguishable encouragement of faculty mentor and assistant professor, Tammy Chang, M.D., M.P.H., M.S. Notably, Dr. Chang recently co-authored a paper with first-year resident Julie Blaszczak, M.D. and medical student Manisha Rai on "Real-Time Data Collection Using Text Messaging in a Primary Care Clinic." The study is available ahead of print online, in the journal Telemedicine and E-Health.
Dr. Chang reflects on her experiences as a mentor and mentee, "One of the main reasons for my success as a physician researcher is due to the amazing mentors I have had throughout my training. Mentoring is also the best part of my job today! Learners at all levels bring energy and creativity as our team works to improve the health of youth across the country." Mentorship is a core value of the research team, as both junior and senior faculty have noted the indispensable relationships they have built as part of their professional growth and success.
Giving credit
Credit for the successful learning and research experiences of the U-M Family Medicine resident-researchers goes first, to the residents, for managing to balance all of their duties and learning with their ventures in clinical research. Secondly, to the leader of the resident research program, Katherine J. Gold, M.D., M.S.W., M.S.. Dr. Gold connected residents to mentors, to resources and training, and advocated for residents as they shared their work with broader audiences. A number of faculty lended their expertise and guidance as mentors, including research professor Zora Djuric, Ph.D., research professor Ananda Sen, Ph.D., assistant professor Thomas O’Neil M.D., biostatistician Melissa Plegue, Justine Wu, M.D., M.P.H., Suzanna Zick, N.D., M.P.H., Jill Schneiderhan M.D., and Tammy Chang, M.D., M.P.H., M.S.. The program was also made possible with the support of: residency director and clinical assistant professor Margaret Dobson, M.D.,assistant residency directors Nell Kirst. M.D., Jean Wong, M.D., and Samuel Romano, Ph.D., Deb Wright, Blythe Bieber, Katie Grode, and so many faculty and staff who provided research consultations and support for the residents and their mentors.
Dr. Gold conducted an institutional-wide study of resident research programs across 22 departments at the University of Michigan. She presented a baseline report at the Health Professions Education Day 2017. The survey identified unmet needs in residency research programs, including funding especially in primary care specialties, increased support for mentors, expertise in statistical and research design, and a better understanding of barriers to research engagement and publication among residents. A PDF of her conference poster is available here.
Do graduating residents go on to publish, present, and pursue research opportunities after leaving U-M? In fact, many do, including former family medicine resident from the class of 2015, Amy Kreykes, M.D. Dr. Kreykes recently published a review with fellow resident class of 2015, Dr. Hetal Choxi, in the Journal of Family Practice. According to Dr. Kreykes, "Dr. [Joel] Heidelbaugh was instrumental in helping Hetal and I find opportunities for publication." Her advice for current family medicine residents who are interested in reaching a broader audience with their clinical expertise, "Start early, be patient, be prepared to go through multiple drafts of corrections and changes. It takes a long time from the day you submit until publication (plan at least a year). Definitely worth it in the long run, though!" We're proud of Amy and all of the residents who have persevered through their first clinical research experience, with the ultimate goal of improving access and care for their patients. And many thanks to all of the mentors, faculty, and staff who continue to support the resident learning experience!
Find additional highlights from the 2016-2017 resident research program from our @umfamilymed Twitter.