
Adhesive small bowel obstructions (ASBOs) in children are one of the most common causes of hospital readmission after abdominal surgery. ASBOs result from bands of scar tissue — also known as ‘adhesions’ — that develop as a normal part of healing and can cause the intestines to stick together or kink after surgery. These adhesions can lead to blockages in the small bowel that, if advanced, can lead to significant problems that may need urgent surgery.
Typically, pediatric patients with ASBO undergo a CT scan to confirm the diagnosis. If the blockage is severe or the intestine is unhealthy, they will need surgery right away to fix the problem. If they don’t need surgery immediately, they will have a nasogastric (NG) tube placed which will suction air and liquid from their stomach and prevent vomiting. Additionally, food will be withheld to rest the bowel. Since they can’t eat, intravenous fluids and often total parenteral nutrition are required.
It’s a wait-and-see approach to assess if they will improve over time without surgery.
“Since surgery predictably leads to more adhesions, and we know that often patients will improve with nonoperative management, this has become the accepted initial approach. However, one issue is the duration of time to decide if a patient needs surgery with this strategy is quite variable," said Dr. K. Elizabeth Speck, Assistant Professor in the Section of Pediatric Surgery.
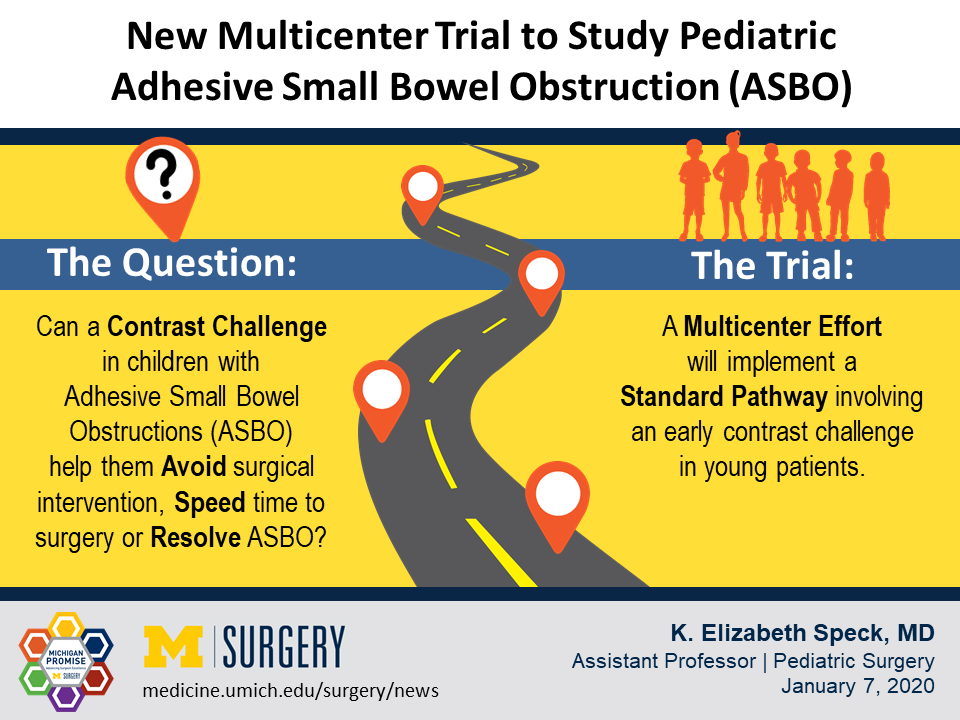
As a collaborator in the Midwest Pediatric Surgery Consortium (MWPSC), Dr. Speck is the primary investigator for the first large-scale, prospective multi-institutional trial assessing ASBO outcomes in children. As its name implies, the Pediatric Adhesive Small Bowel Obstruction (PASBO) trial focuses on children with small bowel obstructions specifically caused by adhesions after surgery.
A gap in data
Unlike children, adults who present with an ASBO are managed with a well-defined and well-studied clinical pathway. They undergo something known as a “Gastrografin challenge.” After their NG tube is placed and their stomach is drained for approximately 48 hours, they receive Gastrografin – a contrast agent that goes into their intestine and lights up on an x-ray. The adult data suggest that a contrast challenge can have diagnostic and therapeutic benefits both by enabling early prediction of those patients who will fail conservative management and thus allow for earlier surgical intervention, and avoidance of surgery in patients who will resolve with non-operative management.
Pediatric surgeons have questioned whether a similar contrast challenge could be safely implemented for children. A few retrospective trials with limited pediatric patients have indicated the answer might be yes and today, a handful of institutions use a contrast challenge in kids. Still, no prospective trial has been performed in children.
"The contrast challenge in adults helps expedite care," said Dr. Speck. "When patients undergo and fail the challenge, they go to the operating room; the surgeons don't have to watch and wait quite as long because it really helps with decision making. We want to be able to do this for our pediatric patients as well, and we believe this trial will help answer a lot of important questions."
Evaluating a standard pathway
Motivated to fill in the gaps in research on pediatric ASBO outcomes, Dr. Speck proposed this prospective, multicenter study to her colleagues in the MWPSC and the group agreed to join. All participating institutions are children’s hospitals where the patients are cared for by Pediatric Surgeons. As part of the study, each institution will implement a standardized algorithm of management that was developed in collaboration between the Pediatric Surgeons and their Pediatric Radiology colleagues. The trial will involve giving an early contrast challenge after a period of stomach drainage. This algorithm is similar to that described in the limited literature for children with ASBOs which was demonstrated to be safe and effective.
There are a number of questions the PASBO trial will seek to answer. The primary question is whether a contrast challenge decreases the likelihood of surgical intervention in children with an adhesive small bowel obstruction. Additionally, the researchers hypothesize that a contrast challenge will decrease the time to the OR for patients who ultimately require an operation, and shorten the overall hospital stay for patients in both groups. Investigators will compare outcomes before and after implementation of the algorithm in a prospective fashion.
Additional dimensions to explore
Another component of this trial is to determine if they can decrease radiation for children with ASBO. Historically, a CT scan has been necessary to evaluate patients with a suspected bowel obstruction. However, the algorithm recommends making the diagnosis using only a two-view abdominal X-ray and utilizing CT scans less often. Long-term outcomes are also an important part of this trial. The investigators will determine if a contrast challenge affects long-term recurrence risk, which is currently an ongoing question in adults as well.
Further, the PASBO trial will examine the cost-effectiveness of varying management strategies.
"A therapeutic effect of the contrast challenge in children could help many avoid surgery, which we hope also improves time to disease resolution, shortens length of stay and lowers costs," Dr. Speck said.
The PASBO trial represents an important step in the management of pediatric ASBO and is expected to start in early to mid-2020. "What we find may really alter the way we care for our pediatric patients not only at the University of Michigan but in children everywhere," Dr. Speck said. "My hope is that, similar to adult data, we'll see that we can decrease the need for operative interventions for adhesive small bowel obstructions while expediting the time to surgery in those patients who need it."
Article by Kim Roth and K. Elizabeth Speck, MD
Downloads

K. Elizabeth Speck, MD
Contact Us
Connect with the Department of Surgery to share your ideas or get in touch.
Department of Surgery
2101 Taubman Center
1500 E. Medical Center Dr.
Ann Arbor, MI 48109
Email: [email protected]
Twitter: @UMichSurgery
