Whether we are caring for our patients, conducting research, or educating medical students, residents, and fellows, our number one priority is to advance the understanding and prevention of cardiovascular disease.
Clinical Care
Our faculty and staff treat patients at Michigan Medicine's Frankel Cardiovascular Center - one of the largest facilities in the heart of the University of Michigan Medical Campus. It is in this 350,000 square-foot, multidisciplinary facility that we can fulfill our vision of being the best academic heart and vascular center in the world.
The facility, which opened June 11, 2007, includes a 24-bed surgical post-procedure ICU, 24 vascular general/moderate care beds, nine cardiac procedure rooms, four cardiac surgery operating rooms, two vascular surgery operating rooms, two general thoracic operating rooms, two endovascular procedure labs, and 36 clinic exam rooms.
Research
Our faculty have made groundbreaking contributions to the prevention and treatment of heart disease. Our research efforts span a broad spectrum of basic, translational, and clinical research activities.
Basic and Translational Research
Our strengths in basic and translational research include:
- Arrhythmia
- Cardiac Myocyte Biology
- Cardiovascular Biomechanics
- Cardiovascular Genetics
- Tissue and Cell Regeneration
- Vascular and Thrombosis Biology
Clinical Research
We are actively involved in clinical research. New medications, devices, surgical procedures, diagnostic tools and prevention strategies need thorough testing before they can become part of routine patient care. We are involved in numerous clinical trials that span our clinical areas.
Education and Training
It is our duty to pass the torch of knowledge on to the next generation and also to share with healthcare professionals around the world what we have learned in the clinic and research lab to further the prevention and treatment of cardiovascular disease.
Our Fellowship Programs offer comprehensive educational curriculum designed to train future leaders in the field of cardiovascular disease. In addition, we offer a variety of continuing medical education courses and seminars taught by our faculty.
Leadership
Interim Chief, John Bisognano, MD, PhD
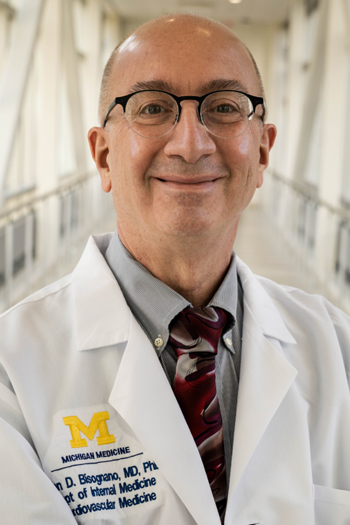
John Bisognano, MD, PhD is a Clinical Professor of Internal Medicine and Interim Chief of the Division of Cardiovascular Medicine. Dr. Bisognano earned his bachelor's degree from MIT, his MA in chemistry and PhD in physical chemistry from SUNY-Binghamton University, and his MD from SUNY-Upstate Medical College. Dr. Bisognano completed his internal medicine residency at the University of Michigan where his interest in cardiology and hypertension was ignited by Dr. Stevo Julius. After completing a fellowship in hypertension, Dr. Bisognano moved to Colorado to complete a fellowship in cardiology and advanced heart failure and transplant at the University of Colorado.
Dr. Bisognano returned to the University of Michigan where he was an Assistant Professor of Internal Medicine for several years before joining the new heart transplant team at the University of Rochester in 2001. While there, he served in numerous leadership roles, including Director of Cardiac Rehabilitation, Medical Director of the University’s Accountable Care organization, and Director of Outpatient Cardiology. In 2021, Dr. Bisognano returned to the University of Michigan and joined faculty in the Division of Cardiovascular Medicine as a clinical professor. He was named the division's interim chief in 2023.
Dr. Bisognano sees patients on the inpatient cardiology services, the inpatient consultative service, and in outpatient clinics. His area of specialty includes general cardiology, as well as severe and resistant hypertension, lipid management, and management of patients with chronic heart failure and ischemic coronary and vascular disease.
A significant part of Dr. Bisognano’s career has been dedicated to general cardiology. He has a longstanding interest in severe and refractory hypertension including device-based therapies for hypertension and is the author of more than 115 journal articles, three books, and numerous book chapters. Dr. Bisognano has served as PI on an NIH R01 grant related to behavioral interventions in people with mild hypertension. He currently serves as co-investigator on an NIH R61/R33 grant for community-based interventions in hypertension.
Dr. Bisognano has served as President of the American Society of Hypertension, Vice-Chair of the American Heart Association Council on High Blood Pressure, Upstate New York State Governor of the American College of Cardiology, and President of the New York Cardiovascular Society.
Dr. Bisognano has been recognized with numerous honors and awards including the University of Rochester Kuhn Teaching Fellowship for Outstanding Medical Student Teaching, the University of Rochester Medical Center Board Excellence Award, and the American Heart Association Arthur J. Moss Award.
Administrator, Joseph Zogaib
Joseph Zogaib
Administrator, Division of Cardiovascular Medicine
1500 E. Medical Center Drive
2722H Cardiovascular Center
Ann Arbor, MI 48109
[email protected]
Faculty Leadership
Keith Aaronson
Professor, Department of Internal Medicine
Director of Adult Heart Transplant
Stanley Chetcuti, MD
Professor, Department of Internal Medicine
Director, Interventional Cardiology
Kim Eagle, MD
Albion Walter Hewlett Professor of Internal Medicine
Professor of Health Management and Policy, U-M School of Public Health
Director, Samuel and Jean Frankel Cardiovascular Center
Director, Cardiovascular Medicine Clinical Quality
James Froehlich, MD
Professor, Department of Internal Medicine
Director, Anticoagulation Services
Director, Vascular Medicine
Hitinder Gurm, MD
Professor, Department of Internal Medicine
Associate Chief Clinical Officer for UH/CVC Services
Scott Hummel, MD
Assistant Professor, Department of Internal Medicine
Veterans Affairs Chief of Cardiology
Todd Koelling, MD
Professor, Department of Internal Medicine
Director, Heart Failure
Theodore Kolias, MD
Professor, Department of Internal Medicine
Director, Echocardiography
Vallerie McLaughlin, MD
Kim A. Eagle MD Endowed Professor of Cardiovascular Medicine,
Department of Internal Medicine
Associate Division Chief
Associate Chief Clinical Officer, UMMG Cardiovascular Services
Director, Pulmonary Hypertension Program
Hakan Oral, MD
Professor, Department of Internal Medicine
Director, Electrophysiology
Contact Us
Academic Office
Administrative Assistant
Department of Internal Medicine
Division of Cardiovascular Medicine
1500 E. Medical Center Drive
2139 Cardiovascular Center
Ann Arbor, MI 48109
[email protected]
Patient Inquiries
- For our clinic information, specialty clinics and programs, procedure information and more, please visit the Michigan Medicine Frankel Cardiovascular Center.
- Michigan Medicine Patient and Visitor Guide



